Positive airway pressure: Making an impact on sleep apnea
Release date: September 1, 2019
Expiration date: August 31, 2022
Estimated time of completion: 0.75 hour
Click here to start this CME activity.
ABSTRACT
Positive airway pressure (PAP) devices deliver a pressurized column of air to open the airway in patients with sleep apnea. For patients with moderate to severe sleep apnea, PAP therapy is the gold standard for treatment, with demonstrated improvements in daytime sleepiness and cardiovascular measures that are superior to conservative treatments. For a variety of reasons, adherence to PAP therapy is a challenge for many patients, resulting in deficits in the frequency and duration of use. To improve use and compliance to therapy, several advanced features are available to enhance comfort, pressure, and humidification factors associated with PAP devices. Patient motivation strategies such as motivational interviews, desensitization protocols, and PAP “NAPs” are also being employed to improve adherence to therapy.
KEY POINTS
- PAP therapy is the gold standard treatment for moderate to severe sleep apnea.
- Adherence to PAP therapy remains a challenge due to the PAP device itself and various patient comfort factors.
- Features of PAP devices that may improve adherence are advanced pressure control, including ramp, auto and bilevel, heated humidification, and compliance data reporting.
- Strategies to motivate patients to use PAP therapy include motivational interviewing, desensitization, and PAP “NAPs.”
PATIENT-CENTERED STRATEGIES TO IMPROVE ADHERENCE
Innovative strategies and approaches focusing on patient factors affecting PAP adherence include motivational interviewing, motivational enhancement, telemedicine, and desensitization techniques.
Motivational interviews and enhancement
Motivational interviewing and motivational enhancement were first used to help with alcohol abuse.17 Motivational interviewing is goal-oriented, patient-centered counseling to elicit a particular behavioral change. The goal is to explore and resolve ambivalence, increase engagement, and evoke a positive response and perspective that builds momentum and results in action.
Motivational enhancement and motivational engagement in the use of PAP therapy were evaluated in the Patient Engagement Study.18 Patients were assigned to usual care (n = 85,358) or active patient engagement (APE) (n = 42,679). Usual care involved diagnosis of apnea, initiation of CPAP, and follow-up, whereas APE included daily feedback (ie, daily scores of apnea–hypopnea index, mask leaks, hours used), positive praise messages, and personal coaching assistance. Overall adherence for patients assigned to APE was 87% compared with 70% in the usual-care group. The hours of use per night also increased for patients in the APE group.
,The Best Apnea Interventions for Research trial randomized patients with or at risk of cardiovascular disease (N = 169) to CPAP alone or CPAP with motivational enhancements for 6 months.19 Motivational enhancements and interventions included brief in-person and phone interventions. An overall average difference of 99 minutes per night improvement in CPAP use was reported in the motivational enhancement group compared with CPAP alone.
The Motivational Interviewing Nurse Therapy study trained nurses in motivational interviewing and randomized 106 patients with newly diagnosed OSA to CPAP alone or CPAP plus motivational interviews.20 Motivational interviews involved 3 sessions: 1 to build motivation prior to the CPAP titration, 1 to strengthen the commitment to achieve the prescribed time, and a booster session 1 month after CPAP setup. Adherence was found to improve at 1, 2, and 3 months in the motivational interview group; however, no difference between the 2 groups in adherence was noted at 12 months.
Telemedicine
The role of telemedicine in improving adherence with CPAP therapy was evaluated in 75 patients with moderate to severe apnea randomized to APAP alone or with phone call support from a research coordinator.21 Phone calls occurred 2 days after device setup, and daily monitoring of several factors was done via modem. Patients were contacted if the mask was leaking more than 30% of the night, use was less than 4 hours per night on 2 consecutive nights, the apnea–hypopnea index was greater than 10, or the average pressure needed was higher than 16 cm of water. Statistically significant improvement was found in the telemedicine group in mean adherence, minutes used per day, and mean amount of time spent with the patients.
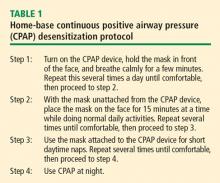
Desensitization to PAP therapy
Case scenario #6
A 33-year-old woman with a history of anxiety and depression and a remote history of abuse as a child was diagnosed with severe apnea. When she tries to use her CPAP, she has a sense of panic and cannot proceed.
Which of the following has NOT been shown to be beneficial in this situation?
- Psychologist for behavioral therapy
- Desensitization protocol
- PAP “NAP”
- Short-acting hypnotics
- None of the above
Answer: Short-acting hypnotics.
The short-acting hypnotic zaleplon (Sonata) was evaluated in a 1-month study of 88 patients compared with placebo control, and no difference was found between the 2 groups in measures of adherence to therapy or symptoms.22
PAP NAP. For some people, at-home desensitization is not enough, and a sleep lab session may be needed. A PAP NAP is a daytime study conducted in the sleep lab. Patients do not necessarily sleep, but work with a technologist with a minimal hookup to polysomnography equipment on mask desensitization, as well as biofeedback techniques. PAP NAPs are indicated for patients with claustrophobia, anxiety surrounding PAP therapy, or pressure intolerance.
A study of 99 patients with moderate to severe apnea and insomnia and concomitant psychiatric disorders resistant to CPAP evaluated adherence in a group receiving a PAP NAP (n = 39) compared with a control group (n = 60).23 The PAP NAP group had marked improvement in completion of CPAP titration in the lab, filling the CPAP prescription, and using CPAP more than 5 days a week and more than 4 hours a night.
A new innovative concept called the Sleep Apnea Patient-Centered Outcomes Network is a collaborative group that includes patients, researchers, and clinicians.24 The group addresses issues such as cost, outcomes, and value in the diagnosis and treatment of sleep apnea. A patient-centered website provides forums, education, and data collection capability for researchers (myapnea.org).
SUMMARY
PAP therapy is the gold standard for treatment of patients with moderate to severe OSA, though poor adherence to PAP therapy is a persistent problem. Advanced features in PAP devices such as APAP and other innovative strategies like motivational enhancement and desensitization protocols and PAP NAP are being used to address poor adherence. More randomized controlled trials are needed to evaluate PAP for sleep apnea.