Obstructive sleep apnea basics
Release date: September 1, 2019
Expiration date: August 31, 2022
Estimated time of completion: 0.75 hour
Click here to start this CME activity.
ABSTRACT
Obstructive sleep apnea (OSA) is a condition caused by repeated episodes of upper airway collapse and obstruction during sleep associated with arousal from sleep with or without oxygen desaturation. OSA is a highly prevalent condition, particularly in individuals with established risk factors and comorbid conditions. Screening for OSA includes a sleep history, review of symptoms, and physical examination, the results of which can identify patients that need testing for OSA. The polysomnogram or home sleep apnea test results aid in the diagnosis of OSA and its severity.
KEY POINTS
- OSA is characterized by repeated episodes of complete or partial obstruction of the airway during sleep.
- The prevalence of OSA is underestimated and underdiagnosed.
- A sleep history, simple upper airway examination, and quick validated screening tool like the STOP-BANG or Epworth Sleepiness Scale aid in identifying the need for testing for OSA.
- Polysomnogram is the gold standard for evaluation of OSA. Home sleep apnea tests can be used to confirm a diagnosis of OSA in patients at high risk for moderate to severe OSA.
DEFINITION
Obstructive sleep apnea (OSA) occurs when there are recurrent episodes of upper airway collapse and obstruction during sleep associated with arousals with or without oxygen desaturations. The oropharynx in the back of the throat collapses during OSA events to cause arousal or oxygen desaturation or both resulting in fragmented sleep.
PREVALENCE
Studies reveal OSA is prevalent. A 2015 study in Switzerland reported 50% of men and 23% of women had at least moderate OSA.1 In 2002, the Sleep Heart Health study found that 24% of men and 9% of women have at least mild OSA.2 In the Wisconsin Sleep Study Cohort, it was reported that 10% of men and 3% of women age 30 to 49 have at least moderate OSA, while 17% of men and 9% of women age 50 to 70 have at least moderate OSA.3 OSA is highly underrecognized and it is estimated that 82% of men and 93% of women in the United States with OSA are undiagnosed.4
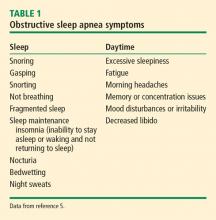
SYMPTOMS
RISK FACTORS
The risk of OSA is influenced by unmodifiable and modifiable factors. Unmodifiable risk factors include male sex, age, and race. Genetic predisposition or a family history of OSA as well as cranial facial anatomy resulting in narrow airways may impart higher risk of OSA. Modifiable risk factors include obesity, medications that cause muscle relaxation and narrowing of the airway (opiates, benzodiazepines, alcohol), endocrine disorders (hypothyroidism, polycystic ovarian syndrome), smoking, and nasal congestion or obstruction.6
Sex
Men are at higher risk for OSA than women although once women reach menopause they have a risk similar to men. Postmenopausal women on hormone replacement therapy were found to have lower rates of OSA, suggesting that loss of hormones results in greater risk of OSA.7,8 Women also have more OSA during rapid eye movement (REM) sleep and less OSA when sleeping supine, whereas most men have OSA when sleeping supine.9,10 OSA is less severe in women compared with men of similar body mass index (BMI).11 Symptoms vary in men and women: snoring and witnessed apneas are more common in men whereas insomnia and excessive daytime sleepiness are more common in women.11 This may account for delayed diagnosis and the higher mortality in women compared with men.
Age
The risk of OSA increases with age. In a study of men 65 or older, the prevalence of moderate OSA was 23% in men younger than 72 and 30% in men older than 80.12 By comparison, the prevalence of moderate OSA in men 30 to 40 years was 10%.3 Increased risk of OSA with age may be due to age-related reduction in slow wave sleep (ie, deep sleep), which is protective against sleep-disordered breathing and airway collapse.13 Older adults are also less symptomatic, reporting less daytime sleepiness and fatigue.14
Race
The Sleep Heart Health Study found a slightly increased risk of moderate to severe OSA in blacks (20%) and American Indians (23%) compared with whites (17%).2 Another study showed the prevalence of OSA was 30% in whites, 32% in blacks, 38% in Hispanics, and 39% in Chinese individuals.15 A higher prevalence of OSA in young blacks (≤ 25 years) compared with whites was reported,16 although another study found no differences based on race in older patients.17 These differences among racial groups may be due to variations in craniofacial anatomy.
Obesity
There is a correlation between increased risk of OSA and obesity (BMI > 30 kg/m2) and its correlates of greater waist-to-hip ratio and neck circumference.2 A 10% increase in body weight results in a sixfold increase in moderate to severe OSA and increases the apnea–hypopnea index (AHI; number of breath pauses or respiratory events per hour) by 32% whereas a 10% decrease in weight decreases the AHI by 26%.18
COMORBIDITIES
OSA is associated with a number of comorbid conditions including stroke, myocardial infarction, hypertension, hyperlipidemia, glucose intolerance, diabetes, arrhythmias including atrial fibrillation, pulmonary hypertension, congestive heart failure, and depression. Patients with moderate or severe OSA are at higher risk of these comorbid conditions.19
Patients with cardiovascular disease have a very high prevalence of OSA: hypertension (83% mild to 30% moderate to severe OSA), heart failure (55% to 12%), arrhythmias (50% to 20%), stroke (75% to 57%), and coronary heart disease (65% to 38%).20 Increased awareness and early diagnosis of OSA is critical to reducing cardiovascular disease burden.