Calcium and vitamin D: To supplement or not?
ARE CALCIUM SUPPLEMENTS SAFE?
Calcium supplements often cause gastrointestinal symptoms, particularly constipation. They have been shown to double the risk of hospital admission due to abdominal symptoms.21 In the absence of clear evidence of benefit, these facts alone should militate against their routine use. Calcium supplements also cause hypercalcemia and hypercalciuria22 and increase the risk of renal calculi (by 17% in the Women’s Health Initiative8).
Over the last decade, evidence has emerged that calcium supplements may also increase the risk of myocardial infarction, and possibly stroke. This finding was not statistically significant in any single study, but is consistently present in meta-analyses.23
Evidence from the Women’s Health Initiative
When studies of calcium with vitamin D are added to these meta-analyses, the results are less consistent. This is because such meta-analyses are dominated by the Women's Health Initiative (because of its large size, with 36,282 participants). There have been 2 different analyses of this trial with respect to cardiovascular events.
,When the Women’s Health Initiative as a whole was analyzed, there was no significant effect of calcium plus vitamin D on vascular end points. However, there is a significant interaction between body mass index and the effect of supplements, such that nonobese women demonstrated a 17% increase in myocardial infarction.24 This study was unusual in that it included women already taking calcium and vitamin D supplements.
There was a significant interaction between baseline use of supplements and the effects of the trial intervention on vascular events, justifying analyzing the supplement-naive individuals separately. In this group of 16,000 women, an increase in clinical myocardial infarction of 22% was found, similar to the findings with calcium supplements alone.25
Thus, there is consistent evidence that introducing a calcium supplement de novo increases the risk of myocardial infarction (Figure 2).16,25–31 We calculate that treating 1,000 patients with calcium or calcium plus vitamin D for 5 years would cause an additional 6 myocardial infarctions or strokes (number needed to harm 178) and prevent only 3 fractures (number needed to treat 302).25
ARE VITAMIN D SUPPLEMENTS EFFECTIVE?
Vitamin D is highly effective in treating osteomalacia, improving symptoms within days and increasing bone density by as much as 50% over 1 year.32,33 In contrast, randomized controlled trials of vitamin D supplements alone in people without osteomalacia have not shown increases in bone density or changes in fracture risk.34–37
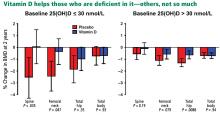
In 2017, my colleagues and I published a trial showing that vitamin D supplementation increases bone density by 2% to 3% in the spine and femoral neck in participants with baseline 25-hydroxyvitamin D levels below 30- nmol/L (12 ng/mL), but those starting above this level showed no effect (Figure 3).38 And a reanalysis of an earlier study confirmed this 30 nmol/L threshold for an effect of vitamin D on bone density.39 The finding of a clear-cut threshold for vitamin D effects is predicted by the physiologic considerations set out above.
Belief that higher levels of 25-hydroxyvitamin D are better is based on observational data. However, correlation does not prove causation, and it is likely that causation is reversed here. Those with better health are likely to spend more time exercising outdoors, are less likely to be obese, and are less likely to have inflammatory conditions; and as a result, they are more likely to have better vitamin D status. We should now be using trial-based definitions of vitamin D deficiency as opposed to thresholds derived from disease associations in observational studies.
Vitamin D supplements have also been suggested to benefit cardiovascular health and to reduce cancer risk, though current clinical trial data provide no support for these hypotheses.36,40 Other trials addressing these questions are ongoing.
ARE VITAMIN D SUPPLEMENTS SAFE?
The safety of vitamin D supplements has generally been assessed with respect to the incidence of hypercalcemia. On this basis, very high doses have been promoted. However, there is now evidence that doses of 4,000 IU/day, 60,000 IU/month, and 500,000 IU/year increase the risk of falls and fractures.41,42
The threshold for bone benefits discussed above (12 ng/mL) is easily exceeded with doses of vitamin D of 400 to 1,000 IU/day. At these levels, vitamin D supplements have no known adverse effects and can be widely endorsed for individuals at risk of deficiency. Supplement doses greater than 2,000 IU/day should be used only in exceptional circumstances, and with appropriate monitoring.
LITTLE USE FOR CALCIUM AND VITAMIN D SUPPLEMENTS
Extensive clinical trials have failed to demonstrate meaningful benefit from calcium supplements in the management of osteoporosis. Calcium supplements are often prescribed in patients who are receiving other treatments for osteoporosis, which may be justified with interventions that have the potential to cause hypocalcemia, but their coadministration with bisphosphonates has been shown to be unnecessary.
Calcium supplements commonly cause gastrointestinal symptoms that are sometimes severe and are likely to contribute to high levels of noncompliance with osteoporosis medications. They increase the risk of kidney stones,8 and there is reasonable evidence to suggest an adverse effect on vascular risk as well.23
Vitamin D deficiency is common in frail elderly people, particularly those with dark skin or living at high latitudes. Low doses of vitamin D are safe and highly effective in preventing osteomalacia. But vitamin D supplements are unnecessary in those who regularly have sun exposure. And high doses of vitamin D have no demonstrated advantage and have been shown to increase the risk of falls and fractures.
Our decision to prescribe calcium and vitamin D supplements should be based on evidence that is of the same quality as for any other intervention we prescribe. Current evidence suggests that there is little reason to prescribe calcium, and that vitamin D should be targeted at those at risk of 25-hydroxyvitamin D levels less than 12 ng/mL.