Optimizing calcium and vitamin D intake through diet and supplements
ABSTRACT
Calcium, a key component of bone, is obtained through diet or supplements, or both, and vitamin D is necessary for normal calcium absorption. Controversy exists as to the efficacy and even the safety of calcium. Our opinion, backed by studies and guidelines, is that adequate amounts of calcium are a must for patients concerned about bone health, and cardiovascular safety is not a concern.
KEY POINTS
- We advise modest targets for total calcium intake, maximizing dietary calcium intake and making up the deficit with calcium citrate supplements.
- Gastrointestinal complaints are common with calcium supplements and can be mitigated with osmotic cathartics (mixed in the same pill or not) or with dose adjustment.
- Vitamin D levels should be optimized to help prevent secondary hyperparathyroidism.
CALCIUM INTAKE IN PATIENTS TAKING ANTIRESORPTIVE DRUGS
Patients often mistakenly think that calcium and vitamin D supplements are given for mild cases of bone loss, and that if their bone loss is significant enough to require a medication, then they no longer need calcium and vitamin D supplements. Most clinical trials showing bone mineral density and fracture benefit from antiresorptive therapy were in patients who were taking enough calcium and vitamin D, so the efficacy of antiresorptive therapy is most clear only when taking enough calcium and vitamin D.34,35
Furthermore, patients with inadequate calcium and vitamin D intake essentially maintain their serum calcium levels by mobilizing calcium from bone; the combination of insufficient calcium intake and administration of agents that interfere with the ability to mobilize calcium from bone may put patients at risk of hypocalcemia.36
OPTIMIZING INTAKE OF CALCIUM AND VITAMIN D
Diet is key to calcium intake. People should consume adequate amounts of calcium-rich foods regardless of whether they have a history of kidney stones, since robust dietary intake of calcium does not increase the risk of cardiovascular disease or kidney stones and may actually have a protective effect. We also remain skeptical of the concern that supplemental calcium increases the risk of cardiovascular disease.
We recommend a target total calcium intake from diet, and if necessary, supplements, of 1,000 to 1,200 mg daily, and not to worry about cardiovascular disease or kidney stones. A patient or clinician reluctant to push calcium intake that high with supplements might opt for a more conservative goal of 800 mg of calcium daily. This recommendation is based on data suggesting that in the presence of vitamin D sufficiency, calcium supplementation with 500 mg of calcium citrate does little for patients whose calcium intake is above 400 mg/day.37
Vitamin D: How much do we need?
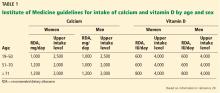
Regarding vitamin D intake, the Institute of Medicine recommends 600 to 800 IU to achieve a 25-hydroxyvitamin D level of 20 to 40 ng/mL.20
The Endocrine Society recommends “at least” 600 to 800 IU, but says that 1,500 to 2,000 IU may be needed to get the 25-hydroxyvitamin D level to 30 to 60 ng/mL.18
The Institute of Medicine based its recommendation on randomized controlled trials that showed fewer fractures with vitamin D intakes of 600 to 800 IU/day.13,14 Also, observational studies show little further reduction in fracture risk when the 25-hydroxyvitamin D levels rise above 20 ng/mL.38 A case-control study found an association between 25-hydroxyvitamin D levels higher than 40 ng/mL and pancreatic cancer.39
The Endocrine Society guidelines recommended higher intakes and levels of vitamin D because there are data suggesting that vitamin D levels higher than 30 ng/mL suppress parathyroid hormone levels further, which should favor less mobilization of bone.40
Levels of 25-hydroxyvitamin D in people exposed to plenty of sunlight rarely go above 60 ng/mL, suggesting 60 ng/mL should be the upper limit of levels to target, and it is unlikely that such levels are harmful.41
Implementing either recommendation—a target 25-hydroxyvitamin D level of 20 to 40 ng/mL or 30 to 60 ng/mL—is reasonable.
CALCULATING A PATIENT’S DIETARY CALCIUM INTAKE
A detailed dietary history can be obtained by a dietitian, or by using the Calcium Calculator app supported by the International Osteoporosis Foundation.43 However, dietary calcium intake can be assessed quickly. To approximate a patient’s total dietary calcium intake (in milligrams), we multiply the number of servings of dietary calcium by 300. A serving of dietary calcium is found in:
- 1 cup of milk, yogurt, calcium-fortified juice, almonds, cooked spinach, or collard greens
- 1.5 ounces of hard cheese
- 2 cups of ice cream, cottage cheese, or beans
- 4 ounces of tofu or canned fish with bones such as salmon or sardines.
Therefore, if a patient consumes 1 cup of milk daily and 1 cup of yogurt 3 times a week, she takes in an estimated 1.5 servings of dietary calcium daily, or 450 mg. What the patient does not receive in the diet should be made up with supplemental calcium.