Perioperative considerations for patients with liver disease
ABSTRACT
In surgical patients with underlying chronic liver disease, surgical outcomes correlate with hepatocellular function. The risk of surgery in such patients should be assessed preoperatively using the Child-Pugh or Model for End-Stage Liver Disease (MELD) severity scoring systems. Patients with severe liver disease (eg, Child-Pugh class C) should not undergo any elective surgery and should be evaluated for liver transplantation. In patients who can proceed with surgery, coagulopathy should be corrected preoperatively and careful fluid management is required intraoperatively to avoid hypotension. Renal insufficiency (as evidenced by elevated creatinine) may indicate that hepatorenal syndrome has developed and carries a poor prognosis.
KEY POINTS
- Patients with acute hepatitis should delay elective surgery until after their hepatitis resolves.
- Patients with chronic liver disease who have developed any index complication—variceal hemorrhage, ascites, hepatic encephalopathy, or jaundice—are at increased risk for postoperative complications and death.
- The Child-Pugh and MELD scores appear to be comparably effective in predicting surgical outcomes in patients with liver disease.
- Cardiac surgery with cardiopulmonary bypass and abdominal surgery are particularly high-risk procedures in patients with liver disease.
- If cholecystectomy is indicated in a patient with compensated liver disease, laparoscopy should be the initial approach, with conversion to an open procedure only if necessary.
Assessing patients with liver disease for surgery is one of the most common reasons for hepatology consultation in the hospital. This review focuses on practical aspects of evaluating patients with known or suspected liver disease and provides guidance for determining whether it is safe to proceed with surgery in such patients. I begin with a case study to introduce some common clinical challenges and then revisit the case—with relevant teaching points—at the end.
CASE: A MIDDLE-AGED MAN WITH LIVER DISEASE SCHEDULED FOR CARDIAC SURGERY
A 57-year-old man with a history of liver disease is referred for preoperative assessment. It is 6:30 pm, and the patient has just arrived in the hospital; he is scheduled for coronary artery bypass graft surgery (CABG) early tomorrow morning for ischemic heart disease. Ten years ago, he was diagnosed with hepatitis C virus infection; 2 years later, he had a cholecystectomy. He has a remote history of intravenous drug use.
The sub-intern asks for an assessment of operative risk as well as advice on the type of anesthesia to be used.
HEPATIC EFFECTS OF ANESTHESIA
Anesthesiologists are keenly aware of the hepatic effects of anesthesia and that they must carefully choose anesthetics for patients with liver disease. There are a number of at least theoretical concerns about using particular anesthetics:
- Inhaled anesthetics, such as isoflurane, cause systemic vasodilation and depress cardiac output. These effects are of concern since many patients with advanced liver disease already have a hyperdynamic circulation because of peripheral vasodilation.
- Spinal or epidural anesthetics may reduce mean arterial pressure, which is of concern for similar reasons.
- Nitrous oxide has less of a depressive effect unless the patient has concomitant hypercapnia.
Another consideration is the hepatic metabolism of anesthetic agents. Use of halothane, which is 20% metabolized by the liver, is now uncommon, particularly if there is any concern about liver disease. In contrast, enflurane is only 4% metabolized by the liver. Numerous other anesthetics—including isoflurane, desflurane, and sevoflurane—have only minimal hepatic metabolism (< 0.2%), which makes them, along with nitrous oxide, the best anesthetic choices for patients with liver disease.
ASSESSING OPERATIVE RISK
The more important issue in the consultation for our patient is the degree of operative risk associated with his underlying liver disease. A number of factors are pertinent, including the etiology and severity of the liver disease and the type of surgery planned.
Acute liver disease has higher operative risk
Literature dating back 40 years has associated acute viral and alcoholic hepatitis with poor outcomes in surgical patients. Major elective surgery for a patient with suspected acute hepatitis A, for example, should be deferred until the patient has recovered, barring some compelling reason for greater urgency, such as a perforated viscus.
In chronic liver disease, hepatocellular function predicts outcome
When a patient with liver disease is evaluated for surgery, evidence should be sought to determine whether an index complication has already occurred. Because the patient in our case study had a cholecystectomy several years before, I would also ask, “What did the surgeon say your liver looked like? Did you have any bleeding problems afterwards? Did you develop ascites?”
It is also important to determine whether portal hypertension is present. For a patient with liver disease, otherwise unexplained thrombocytopenia is a useful indicator of portal hypertension.
Systems for scoring liver disease severity
Even a surgical patient with well-compensated liver disease is at risk for developing complications postoperatively, particularly if abdominal surgery is planned. Risk should be assessed in all patients with liver disease using either the Child-Pugh scoring system or the Model for End-Stage Liver Disease (MELD) scoring system.
The Child-Pugh score, which assigns 1 to 3 points according to the presence/absence and levels of each of five simple factors (bilirubin, albumin, prothrombin time/international normalized ratio [INR], ascites, and encephalopathy stage), has been used for decades to assess the severity of liver disease. Patients with Child-Pugh class A disease (score of 5–6) have well-compensated cirrhosis and good synthetic function, and therefore have essentially no restrictions for undergoing surgery. For patients in Child-Pugh class B (score of 7–9), the risk of perioperative complications and mortality is higher and any major hepatic surgery (such as hepatic resection) should be avoided. Patients with class C cirrhosis (score of 10–15) are not candidates for any major elective surgery and should be considered for liver transplantation referral.
The MELD scoring system was developed more recently and is used to prioritize eligibility for liver transplantation. Calculated using a mathematical formula that incorporates three objective patient variables—
creatinine, bilirubin, and INR—the MELD score correlates very well with prognosis. The score can be calculated by an online MELD calculator such as the one at www.unos.org/resources.2 A patient with a high MELD score is unlikely to survive for more than a few months without liver transplantation; a patient with a low MELD score is likely to survive for at least 12 months. Calculating the MELD score is now one of the first assessments in any patient suspected of having cirrhosis.
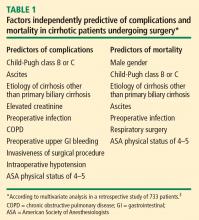
Risk factors for complications and death
In a retrospective study to identify factors associated with complications and mortality in surgical patients with cirrhosis, Ziser et al reviewed the records of 733 patients with cirrhosis who underwent surgical procedures (except liver transplantation) at the Mayo Clinic over an 11-year period (1980–1991).3 The mortality rate within 30 days of surgery was 11.6%. Long-term follow-up showed that most deaths occurred within the first few months after surgery, when many patients succumbed to pneumonia or renal insufficiency.