Prevention of venous thromboembolism after surgery
ABSTRACT
Most surgical patients who require hospitalization are at high risk for venous thromboembolism (VTE) and should receive VTE prophylaxis, usually including pharmacologic prophylaxis. Nevertheless, rates of appropriate perioperative thromboprophylaxis remain stubbornly low, though an expansion in quality-improvement efforts has led to widespread hospital implementation of prophylaxis strategies in recent years. This article reviews important principles and recent developments in perioperative VTE prophylaxis, with a focus on key recommendations and changes in the 2008 update of the American College Chest Physicians’ (ACCP) evidence-based guidelines on antithrombotic therapy.
KEY POINTS
- Effective October 1, 2009, the Centers for Medicare and Medicaid Services is refusing to reimburse for hospital treatment of a primary diagnosis of deep vein thrombosis or pulmonary embolism following recent (within 30 days) hip or knee replacement surgery.
- Mechanical methods of thromboprophylaxis are not effective unless used for at least 18 to 20 hours a day.
- The latest ACCP guidelines recommend extended pharmacologic VTE prophylaxis for up to 28 days in select high-risk patients undergoing general or gynecologic surgery. Extended prophylaxis of varying duration is recommended for patients undergoing major orthopedic procedures.
- Aspirin alone is not recommended for perioperative VTE prophylaxis in any patient group by the ACCP or the International Union of Angiology.
- Patients with renal impairment have fewer anticoagulant options and may require dose adjustment. Weight-based dosing appears to be safe and effective for obese surgical patients.
- New selective and orally administered direct thrombin inhibitors and oral direct factor Xa inhibitors may soon be available for perioperative VTE prophylaxis.
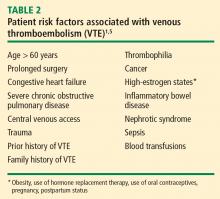
Most surgical patients who require hospitalization should be considered at high risk for venous thromboembolism (VTE) and be given appropriate prophylaxis. For lower-risk procedures such as knee arthroscopy, prophylaxis is needed for those with individual risk factors such as morbid obesity, limited mobility after surgery, or a history of deep vein thrombosis (DVT) or malignancy. Too often, however, prophylaxis is not provided appropriately or not given at all.
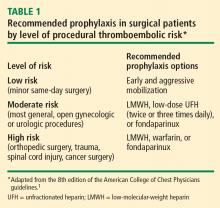
This review surveys the essentials of perioperative VTE prophylaxis and important new developments in the field, which include the 2008 release of new evidence-based clinical practice guidelines on antithrombotic and thrombolytic therapy from the American College of Chest Physicians (ACCP). This 8th edition of the guidelines updates the previous edition, published in 2004, and includes a section by Geerts et al devoted to VTE prevention.1 Other major guidelines are also discussed, as are developments in VTE-related quality measurement, management of special patient populations (those with renal impairment or morbid obesity), and emerging therapies for VTE prophylaxis.
IMPETUS FOR QUALITY IMPROVEMENT IN VTE
A new seriousness about VTE quality measures
The 8th edition of the ACCP guidelines recommends that every hospital develop a formal, active strategy to consistently identify medical and surgical patients at risk for VTE and to prevent VTE occurrence.1 Although prior editions of the ACCP guidelines have made this recommendation for more than 2 decades, fewer than 1 in 10 acute care hospitals had any such strategy in place as recently as 5 years ago. Now, however, most US hospitals have implemented such a strategy, thanks to the growing national emphasis on health care quality measurement in recent years.
The Surgical Care Improvement Project (SCIP) has been at the forefront of this recent quality measures movement. SCIP, a joint project of the American Medical Association and federal government agencies, set a goal to reduce surgical complications in the United States by 25% from 2005 to 2010.2 Two SCIP process measures relate to improving VTE prophylaxis2,3:
- The proportion of surgical patients for whom recommended VTE prophylaxis is ordered
- The proportion of surgical patients who actually receive appropriate VTE prophylaxis within 24 hours before or after surgery.
The Joint Commission and the National Quality Forum recently endorsed these two SCIP performance measures for perioperative VTE prophylaxis along with several others relating to VTE treatment.
CMS raises the stakes with reimbursement restrictions
More significantly, the federal government’s Centers for Medicare and Medicaid Services (CMS) will soon refuse to reimburse for hospital treatment of a primary diagnosis of DVT or pulmonary embolism (PE) following recent (within 30 days) total hip or knee arthroplasty. Effective October 1, 2009, a primary VTE diagnosis following these joint replacement procedures will be added to CMS’ current list of “never events,” or hospital-acquired conditions for which CMS will not provide reimbursement because they are considered the result of preventable medical errors. (Notably, treatment of DVT or PE as a secondary diagnosis will still be reimbursed—for example, if a joint replacement patient develops nosocomial pneumonia, is transferred to the intensive care unit, and then develops VTE.) This addition of DVT and PE to the list is highly controversial since these events sometimes develop even if prophylactic therapy is appropriate and aggressive.
Strategies to promote best practices
In the update for the new 8th edition of its guidelines, the ACCP added recommendations on specific ways for hospitals to identify patients at high risk for VTE and ensure that they receive appropriate prophylaxis. These include the use of computer decision-support systems, preprinted orders, and periodic audit and feedback.1
Researchers at Brigham and Women’s Hospital evaluated the effectiveness of a computer alert system for notifying physicians of newly hospitalized patients at risk for DVT who were not receiving prevention therapy within the first 24 hours of hospital admission.4 These patients presumably “fell through the cracks” and warranted prophylaxis but were otherwise not recognized by the health care team. Risk was determined by a scoring system based on multiple variables, including malignancy, previous DVT or PE, hypercoagulability, major surgery, advanced age, obesity, ordered bed rest, and treatment with hormone replacement therapy or oral contraceptives. Study physicians had to acknowledge having received the alert but could choose whether or not to order VTE prophylaxis. Prophylaxis was used in considerably more patients from the intervention group than from a control group of high-risk patients whose physicians did not receive alerts (34% vs 14%, respectively); accordingly, the risk of a symptomatic DVT or PE event at 90 days was reduced by 41% in the intervention group.
Despite this evidence of improved practice under the alert system, the study begs the question of why the percentage of patients at risk for VTE who were given prophylaxis was still so low (34%), demonstrating how much progress in improving practice remains to be achieved.