The current state of antiplatelet therapy in acute coronary syndromes: The data and the real world
ABSTRACT
Managing antiplatelet therapy for patients with acute coronary syndromes (ACS) is complex, and current therapy options and approaches for these patients are suboptimal. Despite the use of available antiplatelet therapies—aspirin, clopidogrel, and the parenteral glycoprotein IIb/IIIa inhibitors—recurrence of ischemic events in patients with ACS continues to rise over time. Moreover, bleeding remains an important—and often underappreciated—risk with these therapies, and national registries demonstrate that dosing of antiplatelet therapies frequently strays from evidence-based guidelines. Recent quality-improvement initiatives developed in conjunction with national registries of patients with ACS promise to improve adherence to guidelines through hospital-specific performance reports. More evidence-based use of existing and emerging antiplatelet agents has the potential to improve both ischemic and bleeding outcomes in patients with ACS.
KEY POINTS
- Recurrent ischemic events have been observed in all antiplatelet trials to date, in spite of the addition of more potent antiplatelet regimens.
- There appears to be a gradient of benefit from dual antiplatelet therapy depending on patients’ risk of thrombotic events (the greater the risk, the greater the benefit).
- Local practice patterns in interventional therapy for ACS should be taken into consideration when applying results from clinical trials to clinical practice.
- ACS patients who stand to benefit most from antiplatelet therapies also are at the greatest risk of bleeding from those therapies.
- The importance of a tailored approach to antiplatelet therapy and dosing is becoming more widely recognized.
IMPORTANT REAL-WORLD CONSIDERATIONS: BLEEDING AND DOSING
Do not neglect bleeding risk
As antiplatelet therapy becomes more potent in an effort to reduce ischemic events, bleeding risk has become a concern. Major bleeding events occur in more than 10% of patients with ACS receiving antiplatelet therapy,21 although lower rates have been reported in clinical trials in which carefully selected populations are enrolled.7,14,22–24
Major bleeding affects overall outcomes. Major bleeding has clinical significance. The Global Registry of Acute Coronary Events (GRACE), which analyzed data from 24,000 patients with ACS, revealed that major bleeding was associated with significantly worse outcomes: rates of in-hospital death were three times as high—15.3% versus 5.3%—in patients who had major bleeding episodes compared with those who did not (odds ratio = 1.64 [95% CI, 1.18–2.28]).25 The relationship between bleeding and adverse overall outcomes is not fully understood but is nevertheless real and has been observed in multiple databases.
Risk factors for bleeding mirror those for ischemic events. Models are currently being developed to predict bleeding. Unfortunately, the factors that predict bleeding tend to also predict recurrent ischemic events. As a result, patients who stand to benefit most from antithrombotic therapies also are at the greatest risk of bleeding from those therapies.
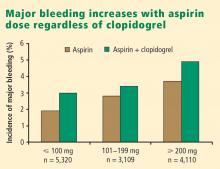
Additive risk from dual antiplatelet therapy. The additional bleeding risk from adding clopidogrel to aspirin is often not fully appreciated. In the CURE trial, the absolute excess risk of major bleeding by adding clopidogrel to aspirin was 1% (3.7% vs 2.7%), which translates to a 35% relative increase compared with aspirin alone.7 In that trial, major bleeding was most prevalent in patients undergoing CABG, and the rate of major bleeding was increased by more than 50% in patients receiving dual antiplatelet therapy when clopidogrel was discontinued 5 days or less before CABG (compared with CABG patients randomized to aspirin alone). This prompted the recommendation that clopidogrel be discontinued more than 5 days prior to CABG.
Similarly, the CHARISMA trial, which used the GUSTO scale for bleeding classification, revealed a significant excess of moderate bleeding with the combination of clopidogrel and aspirin relative to aspirin alone (2.1% vs 1.3%; P < .001) and a nonsignificant trend toward an excess of GUSTO-defined severe bleeding.11
Dosing: Time to end ‘one size fits all’ approach
Dosing of antiplatelet therapies has traditionally been a “one size fits all” strategy, but the importance of tailored therapy and dosing is starting to be realized.
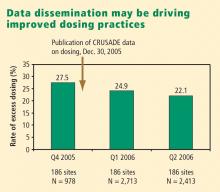
Excess dosing of glycoprotein IIb/IIIa inhibitors is common, dangerous. As an example, the CRUSADE initiative, an ongoing national database of patients with high-risk ACS without ST-segment elevation, showed that 27% of patients treated with glycoprotein IIb/IIIa inhibitors at 400 participating US hospitals in 2004 were overdosed, based on dose-adjustment recommendations in the medications’ package inserts.27 Patients who received excessive doses were significantly more likely to suffer major bleeding than were those who were dosed correctly (odds ratio = 1.46 [95% CI, 1.22–1.73]), an increased risk that was particularly pronounced in women.
Quality-improvement initiatives. The above-mentioned CRUSADE initiative, which was launched in 2001 and involves hundreds of participating US hospitals, has served as a road map for improving dosing practices in antithrombotic therapy. Like the newer ACTION Registry,20 CRUSADE issued performance report cards to its participating hospitals in which antithrombotic medication use over the prior 12 months was compared with each institution’s past performance and with data from similar hospitals across the nation.
SUMMARY AND CONCLUSIONS
Managing antiplatelet therapy for patients with ACS is complex, given the array of medications available and the various combinations in which they can be used. Therapy is likely to become even more complicated, as several new medications are under review by the US Food and Drug Administration or in phase 3 clinical trials.
Current antiplatelet therapy for patients with ACS is suboptimal. Ischemic event recurrence rates continue to rise despite the use of current antiplatelet therapies, bleeding remains an underappreciated risk, and dosing often varies from evidence-based recommendations. Developing prospective strategies for antiplatelet therapy will improve utilization in keeping with a more evidence-based approach. Current ACC/AHA guidelines are the beginning of a roadmap to optimal use of antiplatelet drugs, and quality-improvement initiatives linked to national registries like ACTION promise even more guidance toward optimal therapy through institution-specific benchmarking and performance reports.
Thus far, more effective antiplatelet therapy has led to a greater risk of bleeding. Emerging novel antiplatelet agents and smarter use of existing therapies have the potential to improve both ischemic and bleeding outcomes.