Treatment Options for Stable Chronic Obstructive Pulmonary Disease: Current Recommendations and Unmet Needs
Surgical and bronchoscopic interventions
Surgical and bronchoscopic interventions have the potential to significantly benefit carefully selected patient groups with emphysema.3 LVRS resects parts of the lungs to reduce hyperinflation, and improves lung function and reduces exacerbations in patients with advanced emphysema.3 It can prolong mortality in selected patients,40 but can increase the risk of death in those with low FEV1 and either homogenous emphysema or very low carbon monoxide diffusing capacity.41
Nonsurgical bronchoscopic interventions continue to improve; they have been designed to achieve similar results to LVRS (but with less morbidity), and provide a possible intervention for patients with heterogenous or homogenous emphysema, and significant hyperinflation refractory to optimized medical care.3 Use of endobronchial one-way valves and lung volume reduction coils has resulted in significant improvements in patients’ quality of life, exercise capacity, and pulmonary function for select patients with severe emphysema.42,43 Other therapies, such as adhesives (where a biologic sealant collapses targeted areas of the lung to induce the formation of scar tissue, thus reducing lung tissue volume), and vapor therapy (where heated water vapor is used to deliver thermal energy to the lungs, inducing an inflammatory response that causes contraction fibrosis and atelectasis, and subsequently lung volume reduction) are also in development.44 Consideration of surgical or nonsurgical interventions require referral to a pulmonologist.
Lung transplantation may be an option for patients with very severe COPD without significant comorbidities. Lung transplantation improves quality of life, but does not prolong survival.3,45,46 The procedure is limited by donor availability, high cost, and potential complications.3
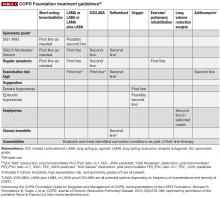
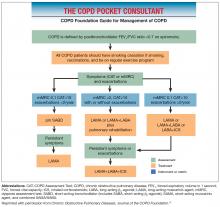
COPD Foundation guidelines
The COPD Foundation guidelines note that some spirometry results are normal, but do not rule out the presence of chronic bronchitis, emphysema, or other lung disease; or are neither normal nor consistent with COPD or other lung disease. The guidelines therefore define 2 additional spirometric grades, referred to as SG 0 (representing patients with normal spirometry) and SG U (representing patients who have a FEV1/FVC ratio >0.7 but FEV1 <80% predicted). At present, neither SG 0 nor SG U are associated with therapeutic options distinct from other spirometric grades, but this may change as we learn more from clinical studies.47,48
Importance of managing COPD comorbidities
Comorbidities are common among patients with COPD, and COPD itself may increase the risk of developing other diseases.3,49-52 It can be difficult to recognize the many comorbidities in patients with COPD, due to the diverse nature of these comorbidities, a lack of understanding of their underlying causes, patients’ failure to recognize or share symptoms, or misdiagnosing them as adverse effects associated with COPD medication.53 Failure to recognize and treat comorbidities can increase risk of hospitalizations or exacerbations, worsen prognosis, increase morbidity, lower the chances of treatment adherence, and place a greater burden on the patient, family, and health care resources.51,52,54-56 Common comorbidities include cardiovascular disease, musculoskeletal dysfunction, metabolic syndrome, anxiety/depression, osteoporosis, lung cancer, and heart failure.3,51,52
The value of effectively managing comorbidities in improving outcomes and adherence to therapy is well documented. For example, personalized management of patients with COPD and comorbid anxiety and/or depression has been shown to reduce both the mental health symptoms and COPD-related outcomes (eg, exercise tolerance, disability).57-59
Comorbidity burden may impact adherence to COPD medication. Depression, for instance, is a known risk factor for nonadherence to treatment. Patients with multiple untreated or uncontrolled comorbid conditions may also be less likely to benefit from pulmonary rehabilitation.60 It is therefore important that comorbidities are managed effectively to improve adherence to therapy, and enhance the benefits of pulmonary rehabilitation.
Patient monitoring
Routine follow-up of patients with COPD is essential as lung function may worsen over time, even with the best available care.3 Worsening of symptoms, activity limitation, and disease progression should be monitored closely to determine when to modify management/pharmacotherapy, and to identify any complications and/or comorbidities that may develop.3 When patients with COPD do not receive the appropriate level of treatment or monitoring, it can be due to: under-reporting of disease severity, symptoms, and exacerbations during consultation; lack of information on the impact of the disease on the patient’s quality of life; and failure to recognize comorbidities.23,25,53 Continued use of the patient questionnaires described previously is recommended, and the GOLD strategy advises that symptoms are assessed at each visit. These follow-up visits also provide an opportunity to monitor patients with COPD for key comorbidities, including heart failure, ischemic heart disease, arrhythmias, osteoporosis, depression/anxiety, and lung cancer, as well as to determine a patient’s current smoking status, taking appropriate action as needed.3