Anxiety and Depression in Chronic Obstructive Pulmonary Disease: Recognition and Management
Diagnosis of anxiety and depression in patients with COPD
The underdiagnosis and undertreatment of anxiety and depression in this population is common and can adversely affect patient outcomes.6,7,9,10,58 Hence, it is crucial that anxiety and depression are identified and more effectively managed in clinical practice.10
Primary care practitioners are the main point of contact for many patients with COPD,6,59,60 and so can play a key role in screening for and early identification of anxiety and depression. However, detection of mood disorders by primary care practitioners is challenging for several reasons. These include the lack of a standardized approach in diagnosis, and inadequate knowledge or confidence in assessing psychological status (particularly given the number of strategies available for screening patients for mood disorders),6 as well as factors associated with time constraints, such as competing agendas, duration of visits, and high patient load.6,61 Furthermore, system-level barriers, such as lack of electronic medical records and adequate health insurance, as well as any communication gaps between primary care and mental health care, may hinder the detection and management of anxiety and depression.6 In addition, patients themselves may have a limited understanding of these comorbidities, or may be hesitant to discuss symptoms of anxiety or depression with their primary care practitioner owing to stigma around mental illness.6
Patients with COPD should be screened and assessed for anxiety and depression, and the United States Preventive Services Task Force recommends that clinicians screen for depression in all adults.6,62 There are several validated screening tools suitable for clinical use:
- Anxiety Inventory for Respiratory (AIR) Disease scale: a brief, easy-to-use tool for screening and measuring anxiety in COPD.63,64 It is a self-administered scale, and takes approximately 2 minutes to complete. The AIR scale is responsive to PR.64
- COPD Anxiety Questionnaire (CAF): a reliable tool for early identification of COPD-related anxiety.65
- Primary Care Evaluation of Mental Disorders (PRIME-MD) Patient Health Questionnaire (PHQ; available at: https://www.phqscreeners.com/select-screener/): the PRIME-MD comprises 26 yes/no questions on the 5 most common psychiatric disorders, including depression and anxiety.66,67 This is not a diagnostic tool, but a high number of positive responses from a patient in any given module indicates that they require further clinical evaluation.
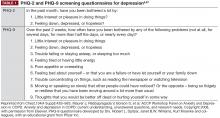
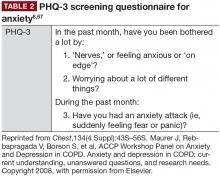
- PHQ-2 and PHQ-9 (Table 1; PHQ-9 available at https://www.phqscreeners.com/select-screener/): widely-used self-administered 2- and 9-item versions of the PRIME-MD, specific to depression; similarly, the 3-item PHQ-3 is available for anxiety assessment (Table 2).6,67,68 In a study investigating tools used by family physicians in England to assess depression, over 75% used PHQ-9.69
- Hospital Anxiety and Depression Scale (HADS) and General Health Questionnaire-version 20 (GHQ-20): both can be used to screen for psychologic distress in patients with COPD.71
- The Beck Anxiety Inventory (BAI) and Beck Depression Inventory (BDI): two 21-item self-report questionnaires that are widely used in the United States to evaluate anxiety and depression.72
In addition to specific anxiety and depression questionnaires (Tables 1 and 2), more general COPD assessments tools, such as the COPD Assessment Test and the COPD Clinical Questionnaire, also incorporate questions that may be indicative of symptoms of these comorbidities in patients with COPD.73
Management of anxiety and depression in COPD
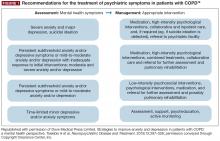
Even though anxiety and depression are among the most common and burdensome comorbid conditions in COPD, less than one-third of patients with these comorbidities receive effective intervention.6,10 Primary care providers have an excellent opportunity to impact this care gap.
As in non-COPD patients, comorbid depression and anxiety may be treated with nonpharmacologic and/or pharmacologic interventions (Figure 1).76