Having the COURAGE to include PCI in shared decision-making for stable angina
Invented by Andreas Grüntzig in 1977, percutaneous coronary intervention (PCI) has revolutionized the management of coronary artery disease.1 Initially, PCI was more attractive than conventional revascularization with coronary artery bypass grafting because it was less invasive, but as time went on PCI acquired its own evidence base of improved clinical outcomes. In fact, for ST-elevation myocardial infarction, non-ST-elevation myocardial infarction, and cardiogenic shock, there is clear evidence that PCI saves lives in both the short and long term.2,3
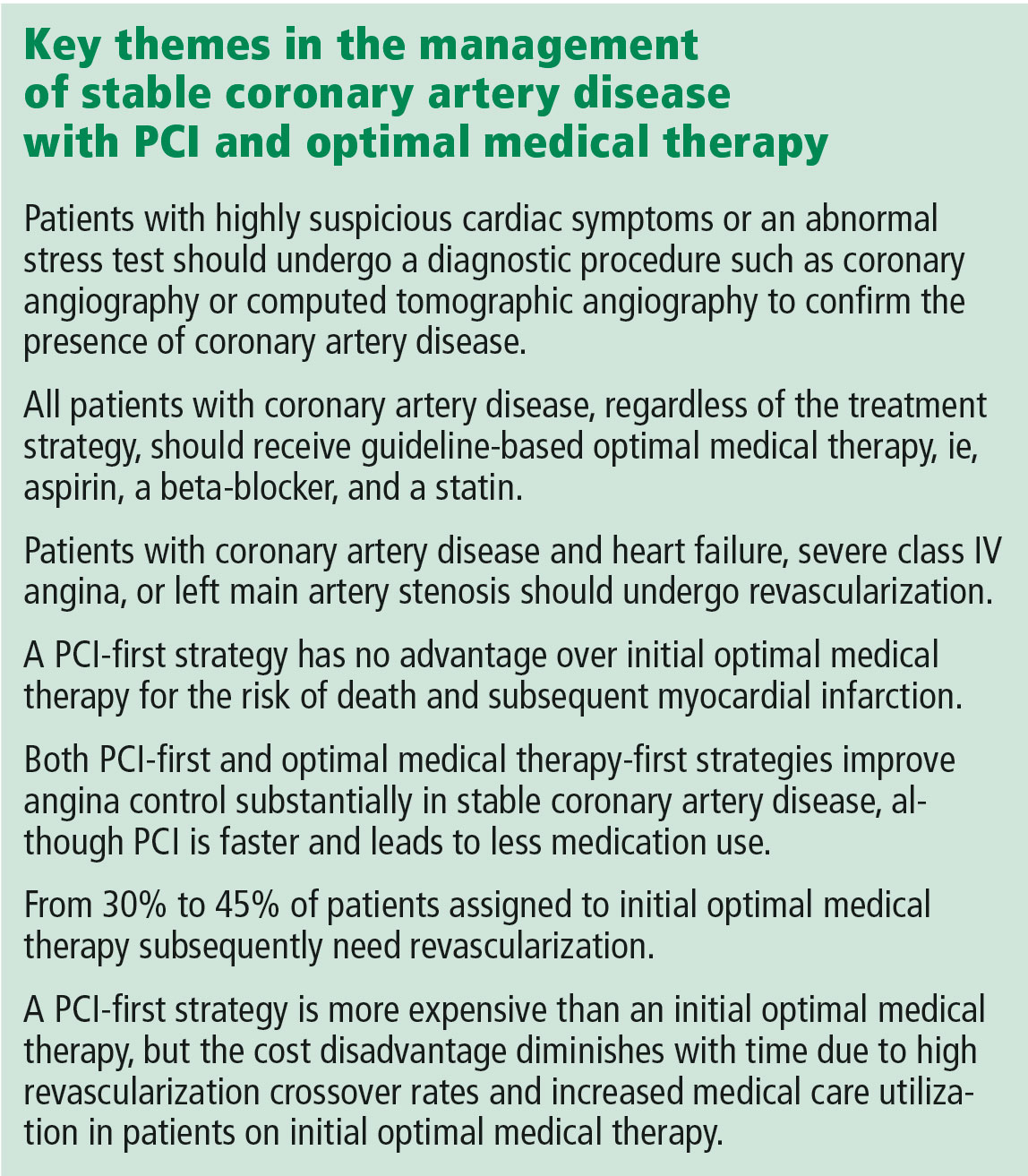
But PCI is also used widely in stable coronary artery disease, and in contrast to the clear-cut benefit in the acute conditions noted above, a series of reports culminating in the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial has shown that PCI in stable coronary artery disease does not reduce the risk of death or of subsequent myocardial infarction.4,5 Cardiologists have heeded the COURAGE trial findings in their clinical decision-making, and the rate of PCI for stable coronary artery disease dropped by 60% from 2006 to 2011.6
In an article in this issue,7 Dr. Michael Rothberg describes a 55-year-old man who develops new-onset angina and then undergoes a Bruce protocol stress test that is stopped at 6 minutes due to chest pain and ST-segment depression. Dr. Rothberg argues that, based on COURAGE trial data, this patient and other patients with stable coronary artery disease should not be treated with PCI but instead should receive optimal medical therapy.
KEY ISSUES ABOUT THE COURAGE TRIAL
To understand the applicability of the results of the COURAGE trial to patient care, it is important to examine a number of key issues about this trial.
First, COURAGE enrolled a narrow group of patients with stable coronary artery disease and excluded many common patient subgroups, such as those with heart failure, severe anginal symptoms, or left main artery stenosis, who would benefit from revascularization.5 Specifically, for every 100 patients enrolled in COURAGE, 161 were excluded for having heart failure, 39 were excluded for class IV angina, and 31 were excluded for left main stenosis.
Second, although COURAGE has been described as a trial of PCI vs optimal medical therapy, it was not. Rather, it was a trial of optimal medical therapy with PCI first vs optimal medical therapy with crossover PCI if medical therapy failed.5 The crossover rate was not insubstantial: 16.1% of the patients in the medical therapy group underwent PCI by the end of the first year, increasing to 32.6% at a median of 4.6 years of follow-up.5,7 And patients with more intense and frequent angina and resulting worse quality of life were the ones who required crossover PCI.8
Third, it has been proposed that patients with suspicious cardiac symptoms or abnormal stress test findings can be managed with optimal medical therapy initially, based on the COURAGE findings. However, the COURAGE trial required diagnostic angiography both to confirm underlying coronary artery disease and to exclude left main disease.5 Thus, regardless of one’s position on the role of PCI in stable coronary artery disease, diagnostic investigation by cardiac catheterization or computed tomographic angiography to confirm the presence or absence of coronary artery disease remains mandatory.
Fourth, optimal medical therapy was prescribed by the trial’s protocol, so that one would expect that both treatment groups received similar levels of optimal medical therapy. However, the optimal medical therapy group required more medications to achieve the same outcome as the PCI group.5
Finally, although it has been reported that the COURAGE trial showed no benefit for PCI, in fact, for the outcome of symptom relief, initial PCI was clearly superior to optimal medical therapy beginning at 3 months and extending out to 24 months—a result for which the magnitude of benefit is underestimated due to the occurrence of crossover PCI.9 In particular, women and patients with a high frequency of angina derived improvement in angina-related quality of life from PCI compared with optimal medical therapy.8,10