Aortic replacement in cardiac surgery
ABSTRACT
The number of aorta procedures performed annually in the United States has grown substantially during the past decade. Cleveland Clinic is a leader in research on the risk of aortic dissection in patients with a bicuspid or tricuspid aortic valve and associated aneurysm, which has led to changes in the recommendations of when to operate. Safety and efficacy data support more proactive treatment for most patients with thoracic aortic aneurysm and/or dissection with a growing emphasis on the need to provide life-long care to patients with aortic conditions.
KEY POINTS
- Adding a proximal thoracic aortic procedure to cardiac surgery does not adversely affect safety and efficacy.
- Presence of a bicuspid aortic valve does not significantly affect outcomes of aortic root procedures.
- Data support aortic replacement in patients when the aortic root vessels reach 5.5 cm in diameter.
- Use of circulatory arrest does not directly affect the stroke risk associated with ascending aortic replacement surgery, but it may be a marker for more serious pathology.
In 2015, Cleveland Clinic cardiac and vascular surgeons performed more than 1,000 open or endovascular operations involving the thoracic aorta, the most of any US medical center. Cardioaortic operations account for a large volume of the procedures performed annually in the Department of Thoracic and Cardiovascular Surgery at Cleveland Clinic. Of the approximately 4,000 cardiac procedures performed per year at Cleveland Clinic, nearly 1 in 5 includes thoracic aorta replacement.
Providing optimal care to patients with thoracic aortic disease requires a multidisciplinary approach beginning in the preoperative phase and extending through the life of patients and their families. In the Aortic Center at Cleveland Clinic Heart & Vascular Institute, cardiovascular medicine and imaging specialists, geneticists, and cardioaortic and vascular surgeons work in unison to provide the highest quality care. This involves active analysis of outcomes to continuously improve the quality of care provided.
This paper examines trends in the treatment of thoracic aortic disease, describes the different types of therapeutic procedures, and explores details about their safety and efficacy by summarizing the key research findings on cardioaortic procedures published from our Center during the last 2 years.
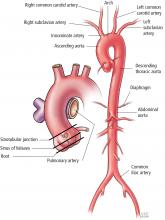
SEGMENTAL PERSPECTIVE
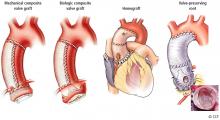
1. Modified Bentall procedure with a mechanical composite valve graft (CVG)
2. Modified Bentall procedure with a biologic CVG
3. Homograft, or allograft, root replacement with a human cadaveric aorta
4. Valve-preserving aortic root replacement with a prosthetic graft but which leaves the patient’s native aortic valve intact with or without accompanying repair of that valve.
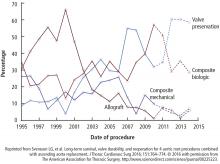
A Cleveland Clinic study published in 2016 analyzed 957 elective aortic root replacement procedures performed from 1995 through 2014.1 The number of procedures in this study were evenly distributed across these 4 aortic root replacement strategies.
The perioperative mortality rate was 0.73% and the stroke rate was 1.4%. For 3 of the 4 procedure types, 15-year survival rates were excellent: above 80% for mechanical CVG, allografts, and valve-preservation surgery. The survival rate for biologic CVG was lower (57%), reflecting the difference in population, as these were typically older patients.
This study also demonstrated the durability of these operations, with a reoperation rate of approximately 15% at 15 years. Reoperation rates for patients having undergone these operations should be considered in the light of competing risk of death from other causes. As such, the risk of reoperation after mechanical CVG, biologic CVG, and valve-preserving procedures were similar, ranging from 5% to 15%. Allografts had the highest reoperation rates (approximately 30% at 15 years) because they used to be the biologic root replacement of choice for younger patients but have since been found to wear out at a similar rate as other bioprostheses.2 As a result, they are now used less frequently for elective indications.
Cleveland Clinic practitioners now perform more than 80 valve-preserving root replacement operations per year, approximately 700 overall.
Clinical implications
For patients presenting with aortic root aneurysm, consider the following:
- Valve-preserving aortic root replacement is preferred for patients with root aneurysm and a tricuspid aortic valve without valve stenosis.
- Valve-preserving aortic root replacement with either remodeling or reimplantation is also preferred for patients with a bicuspid aortic valve with a dilated annulus or root aneurysm, but without aortic-associated aortic valve stenosis
- Mechanical CVG is preferred for younger patients with root aneurysm and aortic valve stenosis (usually a bicuspid or unicuspid aortic valve); biomechanical CVG is preferred for older patients with root aneurysm and associated aortic valve stenosis.
- Allografts are now reserved primarily for patients with endocarditis and for older patients with a small aortic root.