Improving the safety and efficacy of robotically assisted mitral valve surgery
ABSTRACT
To improve outcomes with robotically assisted mitral valve surgery, Cleveland Clinic conducted a study evaluating outcomes in 1,000 consecutive cases. Primary areas of interest were to determine whether increased surgical experience with robotic techniques improved outcomes and to identify opportunities that could improve procedural processes. Results showed that these surgeries were effective and safe in terms of improvements in procedure time, transfusion rates, stroke risk, number of mitral valve replacements, and number of conversions to sternotomy. The development and implementation of a patient-selection algorithm halfway through the study further improved outcomes by refining patient eligibility criteria. This study showed that use of a focused preoperative assessment with an algorithm-driven patient selection process combined with increased technical expertise can enhance outcomes with robotic mitral valve surgery.
KEY POINTS
- Surgeon competence with robotic techniques, which can be improved through experience, is a key to improving outcomes.
- This patient-selection algorithm provides an evidence-based approach to identifying patients who are the best candidates for the robotic approach.
- This study showed that increased surgical competence and improved patient selection improved patient outcomes for the primary end points.
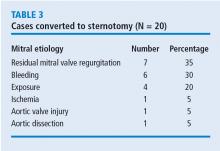
In the years since the introduction of robotically assisted mitral valve surgery, surgeons have looked for ways to improve techniques and procedures. A study from Cleveland Clinic presented at the American Association for Thoracic Surgery in 2016 assessed efficacy and safety outcomes associated with 1,000 consecutive robotically assisted mitral valve surgeries at Cleveland Clinic.1 The purpose of the study was to assess the clinical outcomes from these cases and analyze whether the outcomes changed over time as surgeons became more competent with robotic techniques. This analysis was also designed to identify procedural processes that improved outcomes during the trial.
STUDY METHODS
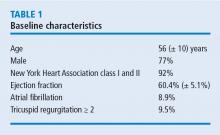
Nearly all cases (96%) were classified as degenerative mitral valve disease (N = 960). Of those, most had posterior leaflet prolapse (68%), about one-third (29%) had bileaflet prolapse, and only 3% had anterior leaflet involvement.
All surgeries were performed through right port incisions and used femoral cannulation for peripheral bypass. The aorta was occluded with either a Chitwood transthoracic clamp or a balloon.
STUDY RESULTS
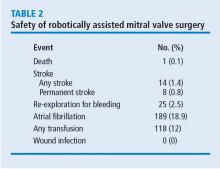
It is important to remember that with femoral artery perfusion, the blood flow is opposite to the normal direction; thus, it goes up the aorta into the head vessels, which presents its own risks and challenges. Also, during retrograde perfusion, there is a risk of dislodging atherosclerotic plaque leading to brain embolus and stroke.
In these 1,000 cases, 997 were planned mitral valve repairs, 2 were mitral valve replacements, and 1 was resection of a mitral valve fibroelastoma. Results for the mitral valve repairs were excellent, with postoperative mitral regurgitation occurring in less than 1% of patients.