CABG: A continuing evolution
ABSTRACT
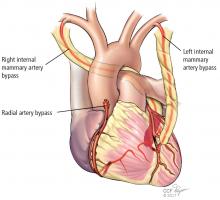
Use of coronary artery bypass grafting (CABG) has had a resurgence, as clinical trial data emerged showing that it remains the standard of care for patients with complex lesions. Debate exists regarding various factors, including endoscopic vs open vein-graft harvesting, single vs bilateral mammary artery grafts, radial artery vs saphenous vein grafts, right internal mammary artery vs radial artery grafts, and on-pump vs off-pump surgery. More recent developments include minimally invasive approaches, robotics, and hybrid revascularization, which are changing the risk-benefit ratio for this patient population.
KEY POINTS
- CABG is considered the standard of care for patients with intermediate or high coronary artery disease burden.
- Traditional CABG performed via median sternotomy with the use of cardiopulmonary bypass is the technical standard for surgical coronary revascularization.
- Suturing the left internal mammary artery directly to the left anterior descending artery is the most effective technique for coronary revascularization.
- Minimally invasive approaches to CABG are safe and effective alternatives in select patient populations.
COMPARING CONDUIT OPTIONS FOR CABG
Arterial vs venous grafts
The 1986 report by Loop and colleagues from Cleveland Clinic showed that the patency of the mammary artery graft was superior to that of the saphenous vein and that patients receiving a mammary bypass had significantly better 10-year survival (82.6% vs 71.0%, respectively; P < .0001).13 The findings of this landmark study established the LIMA-to-LAD bypass as the technical standard for surgical coronary revascularization.
Single vs bilateral mammary artery grafts
In December 2016, results of the Arterial Revascularization Trial (ART) were published comparing single vs double mammary artery grafts.14 In this prospective randomized trial, the 5-year results showed no significant difference between these mammary grafts in terms of all-cause mortality, MI, or stroke. Bilateral mammary artery grafts, however, were associated with a higher risk of sternal wound complications (3.5% vs 1.9%, respectively; P = .005) and sternal reconstruction (1.9% vs 0.6%; P = .002).
Radial artery vs saphenous vein grafts
In the largest randomized study comparing these two graft options,16 the 1-year results showed no difference in graft patency; a follow-up analysis is in progress. In contrast, randomized studies from Canada17 and the United Kingdom18 suggest that there are potential benefits associated with use of radial artery grafts in terms of patency and clinical outcomes. In addition, observational data from centers experienced in radial artery grafting have demonstrated favorable outcomes. Radial arteries perform best when bypassing totally occluded or severely stenotic vessels in which there is no or little risk of competitive flow from the native circulation.
Right internal mammary vs radial artery grafts
A propensity-matched comparison study looking at multiple studies (N = 15,374 patients) concluded that use of the right internal mammary artery provides better outcomes.19 It was associated with a 25% risk reduction for late death and a 63% risk reduction for repeat vascularization, both statistically significant vs the radial artery rates. But there is a randomized study showing that the radial artery is as good as or better than the right internal mammary artery. At this point, it is not clear which artery is better as an adjunct for the LIMA-to-LAD bypass.
GUIDELINES FOR GRAFT SELECTION
In 2016, the Society of Thoracic Surgeons published guidelines that encouraged the use of arterial grafts, giving it a class IIa designation, meaning that the evidence indicates it is reasonable to consider.20
The guidelines note the following:
- The internal mammary artery should be used to bypass the LAD when bypass of the LAD is indicated.
- As an adjunct to the left internal mammary artery, a second arterial graft (the right internal mammary artery or radial artery) should be considered in appropriate patients.
- Use of bilateral internal mammary arteries should be considered in patients who are not at high risk for sternal complications.
COMPARING SURGICAL APPROACHES
Traditional CABG performed via median sternotomy and with the use of cardiopulmonary bypass remains the technical standard in surgical coronary revascularization. However, technologies have allowed surgeons to use different and sometimes less invasive approaches that may have good outcomes in select patients with suitable risk profiles and favorable coronary anatomies.
On-pump vs off-pump CABG
The popularity of CABG without cardiopulmonary bypass (“off-pump”) peaked in 2002, when it constituted approximately 23% of CABG procedures and then declined to 17% by 2012.21 The ROOBY (Veterans Affairs Randomized On/Off Bypass) trial of 2,203 VA patients showed that at 1 year, those in the off-pump group had worse composite outcomes, poorer graft patency, and greater incidence of incomplete revascularization than the on-pump group.22 However, the use of off-pump CABG was vindicated in two other trials—CORONARY and GOPCABE—in which experienced surgeons in high-volume centers with high-risk patients had no difference in outcomes at 1 and 5 years.23–25 The recommendation is to tailor the procedure to the patient rather than the patient to the procedure. The best option is always to do what is right for the patient. For example, patients with diseased ascending aortas or liver disease may benefit from an off-pump approach.