Patients with challenging behaviors: Communication strategies
ABSTRACT
Some patients have behaviors that make interactions unpleasant, sometimes contributing to suboptimal outcomes and physician burnout. Understanding common difficult personality types can help doctors plan effective strategies for dealing with each, resulting in more effective communication, less stress, and better health outcomes.
KEY POINTS
- Patients who intensely question everything need validation of their need for information and a collaborative approach based on sound medical evidence.
- Patients whose behavior is hostile and demanding need limits placed on aggressive behavior and assurance that the healthcare team is working in their best interests.
- Patients who seek reassurance to the point of overuse of the doctor’s time need to have boundaries set.
- Many patients who injure themselves and deny the problem have a personality disorder. They need empathy and a clear plan for care, often involving behavioral therapy.
- Physicians should plan effective communication strategies for difficult patients, discuss issues with colleagues, and use relaxation methods to help avoid burnout.
HOW TO STAY IN CONTROL AND IMPROVE INTERACTIONS
Patients with challenging behaviors will always be part of medical practice. Physicians should be aware of their reactions and feelings towards a patient (known in psychiatry as countertransference), as they can increase physician stress and interfere with providing optimal care. Finding effective ways to work with difficult patients will avoid these outcomes.
Physicians also feel loss of control
Most physicians are resilient, but they can feel overwhelmed under certain circumstances. According to Scudder and Shanafelt,33 a physician’s sense of well-being is influenced by several factors, including feelings of control in the workplace. It is easy to imagine how one or more difficult patients can create a sense of overwhelming demand and loss of control.
These tips can help maintain a sense of control and improve interactions with patients:
Have a plan for effective communication. Not having a plan for communicating in a difficult situation can contribute to loss of control in a hectic schedule that is already stretched to its limits. Practicing responses with a colleague for especially difficult patients or using a team approach can be helpful. Remaining compassionate while setting boundaries will result in the best outcome for the patient and physician.
Stop to analyze the situation. One of the tenets of cognitive-behavioral therapy is recognizing that negative thoughts can quickly take us down a dangerous path. Feeling angry and resentful without stopping to think and reflect on the causes can lead to the physician feeling victimized (just like many difficult patients feel).
It is important to step back and think, not just feel. While difficult patients present in different ways, all are reacting to losing control of their situation and want support. During a difficult interaction with a patient, pause to consider, “Why is he behaving this way? Is he afraid? Does he feel that no one cares?”
When a patient verbally attacks beyond what is appropriate, recognize that this is probably due less to anything the physician did than to the patient’s internal issues. Identifying the driver of a patient’s behavior makes it easier to control our own emotions.
Practice empathy. Difficult patients usually have something in their background that can help explain their inappropriate behavior, such as a lack of parental support or abuse. Being open to hearing their story facilitates an empathetic connection.
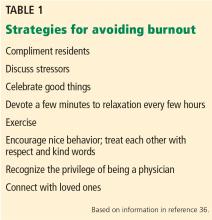
AVOIDING BURNOUT
Discuss problems
Sadly, physicians often neglect to talk with each other and with trainees about issues leading to burnout, thereby missing important opportunities for empathy, objectivity, reflection, and teaching moments.
Lessons can be gleaned from training in psychiatry, a field in which one must learn methods for working effectively in challenging situations. Dozens of scenarios are practiced using videotapes or observation through one-way mirrors. While not everyone has such opportunities, everyone can discuss issues with one another. Regularly scheduled facilitated groups devoted to discussing problems with colleagues can be enormously helpful.
Schedule quiet times
Mindfulness is an excellent way to spend a few minutes out of every 3- to 4-hour block. There are many ways to help facilitate such moments. Residents and students can be provided with a small book, Mindfulness on the Go,37 aimed for the busy person.
Deep, slow breathing can bring rapid relief to intense negative feelings. Not only does it reduce anxiety faster than medication, but it is also free, is easily taught to others, and can be done unobtrusively. A short description of the role of the blood pH in managing the locus ceruleus and vagus nerve’s balance of sympathetic and parasympathetic activity may capture the curiosity of someone who may otherwise be resistant to the exercise.
Increasingly, hospitals are developing mindfulness sessions and offering a variety of skills physicians can put into their toolbox. Lessons from cognitive-behavioral therapy, dialectical behavior therapy, imagery, and muscle relaxation can help physicians in responding to patients. Investing in communication skills training specific to challenging behaviors seen in different specialties better equips physicians with more effective strategies.