Diabetes control during Ramadan fasting
ABSTRACT
For diabetic patients, fasting during Ramadan, the ninth month of the Islamic calendar, can cause wide fluctuations in blood sugar levels, posing a medical challenge for patients and physicians and increasing the risk of acute metabolic complications including hypoglycemia, hyperglycemia, diabetic ketoacidosis, dehydration, and thrombosis. Proper patient education, risk stratification, and modification of antidiabetic medications can reduce the risk of complications.
KEY POINTS
- A diabetic patient who develops signs or symptoms of hypoglycemia during Ramadan fasting should break the fast to avoid serious complications.
- Management of complications in diabetic patients during Ramadan is similar to that for nonfasting diabetic patients. Complications include hypo- and hyperglycemia, diabetic ketoacidosis, and dehydration.
- A common misconception among patients is that pricking the finger for blood sugar testing during fasting hours breaks the fast; this should be addressed during Ramadan-focused diabetes education.
An estimated 50 million patients with diabetes worldwide practice daily fasting during Ramadan, the ninth month of the Islamic calendar, which lasts 29 or 30 days. In the United States, Ramadan begins this year at sundown on Friday, May 26, and ends at sundown on Sunday, June 25.
According to the Multi-Country Retrospective Observational Study of the Management and Outcomes of Patients With Diabetes During Ramadan, conducted in 13 countries, 94.2% of Muslim diabetic patients fasted at least 15 days, and 67.6% of these fasted every day.1
The daily fasting period, which may extend from 14 to 18 hours, starts before sunrise and ends after sunset. The meal taken before sunrise is called Suhur, and the meal after sunset is called Iftar. The fast requires abstaining from eating, drinking, sexual activity, medications, and smoking. For diabetic patients, this poses medical challenges, increasing the risk of acute metabolic complications.
The goal of caring for diabetic patients during Ramadan fasting is to help them to fast without major complications and to empower them to modify their lifestyle in order to achieve this goal.
POSSIBLE METABOLIC COMPLICATIONS
Metabolic complications during Ramadan fasting include hypoglycemia, hyperglycemia, diabetic ketoacidosis, dehydration, and thrombosis.
Hypoglycemia
For patients with type 1 diabetes, fasting increases the risk of hypoglycemia 4.7 times, and the risk is 7.5 times higher for patients with type 2 diabetes.2 However, this is often underreported, as mild to moderate hypoglycemia does not usually require medical assistance.
Precipitating factors include long fasting hours, missing the Suhur meal, and failure to modify drug dosage and timing.
Hyperglycemia
The risk of severe hyperglycemia during fasting is 3.2 times higher in patients with type 1 diabetes and 5 times higher in those with type 2 diabetes.2 Precipitating factors include lack of diet control during the Iftar meal and excessive reduction in the dosage of diabetes medications due to fear of hypoglycemia.
Diabetic ketoacidosis
Ketoacidosis can be precipitated by a lack of diet control during the Iftar meal, excessive reduction in the dosage of insulin due to fear of hypoglycemia, acute stress, and illness or infection.
Dehydration and thrombosis
Patients can become dehydrated during long fasting hours in especially hot weather, by sweating during physical activity, and by osmotic diuresis in poorly controlled diabetes.
Diabetes is a procoagulant condition, and dehydration increases the risk of thrombosis.
OVERALL MANAGEMENT GOALS DURING RAMADAN FASTING
Important aspects of managing diabetes during Ramadan fasting are:
- The pre-Ramadan evaluation and risk stratification
- Promoting patient awareness with Ramadan-focused diabetes education
- Providing instruction on dietary modification
- Modification of the dosage and timing of diabetes medication
- Encouraging frequent monitoring of blood glucose levels
- Advising the patient when to break the fast
- Managing complications.
PRE-RAMADAN MEDICAL EVALUATION AND RISK STRATIFICATION
All diabetic patients who fast during Ramadan should undergo an evaluation 1 or 2 months before the start of Ramadan to determine their level of diabetes control and the presence of acute and chronic complications of diabetes and other comorbid conditions. Also important is to determine the patient’s social circumstances, ie, knowledge about diabetes, socioeconomic factors, religious beliefs, educational status, diabetes self-management skills, and family support in case of hypoglycemia or complications.
The evaluation helps to determine the patient’s risk of diabetes-related complications from Ramadan fasting, which is categorized as very high, high, or moderate/low according to the criteria of the International Diabetes Federation (Table 1).3 Patients should be advised as to the feasibility of fasting based on this risk categorization.
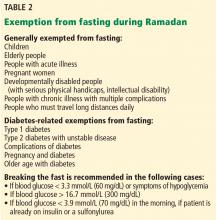
Even though the recommendation is to avoid fasting if the risk is very high or high, many patients fast. But patients should be advised about Islamic regulations exempting people from fasting (Table 2).4
RAMADAN-FOCUSED DIABETES EDUCATION
Improving the patient’s awareness of the risks of Ramadan fasting reduces the chance of complications. Education should include information on diet and exercise, changes in the timing and dosing of medications, signs and symptoms of hypoglycemia and hyperglycemia, the importance of monitoring blood glucose levels on fasting days, and the importance of breaking the fast in case of complications.5