Assessing a multidisciplinary survivorship program in a group of predominantly Hispanic women with breast cancer
Background The prevalence of long-term mental and physical illness is significant among many breast cancer survivors. We have previously reported that Hispanic survivors of breast cancer have a diminished mental and physical health-related quality of life (QoL), though in general, there is a paucity of data for this population and other minorities. Implementing a cancer survivorship program as an integral component of care during and after treatment could improve long-term QoL in survivors of breast cancer and empower them in the transition from treatment to survivorship.
Objective To determine the value of implementing a multidisciplinary survivorship program that includes psychological counselling and interventions based on mindfulness and counselling.
Methods Survivors of stages I-III breast cancer were recruited within 5 years of their diagnosis at an institution in El Paso, Texas, where the majority of patients are of Hispanic ethnicity, to participate for a year in a multidisciplinary program that provided psychological counselling in conjunction with oncology care, dietary advice, and an 8-week course based on mindfulness-based stress reduction. Self-administered questionnaires - the Patient Health Questionnaire-9 for depression, the General Anxiety Disorder-7, and the Short-Form Health Survey-36 (version 2) for QoL - were completed at baseline and every 3 months for 12 months.
Results 94 patients, of whom >90% were Hispanic, were included in this 12-month analysis. 60 patients (63.8%) completed all follow-ups at 12 months. Significant improvement from baseline was observed for patient health and anxiety measures for all ethnic groups combined.
Limitations Small, single-center study; no control arm using other possible interventional methods
Conclusion All breast cancer survivors who participated in this 12-month multidisciplinary interventional survivorship program reported less anxiety and depression, compared with baseline measurements and showed a trend toward improved Mental Component Summary of QoL. We believe these findings are representative of outcome in Hispanic women since >90% of participants were Hispanic.
Funding Cancer Prevention and Research Institute of Texas (CPRIT)-RP120528
Accepted for publication January 4, 2017
Correspondence Safa Farrag, MD; safa.farrag@ssmhealthx.com
Disclosures The authors report no disclosures/conflicts of interest.
Citation JCSO 2017;15(4):e208-e216
©2017 Frontline Medical Communications
doi https://doi.org/10.12788/jcso.0322
Related articles
Posttreatment survivorship care needs of Spanish-speaking Latinas with breast cancer
A qualitative exploration of supports and unmet needs of diverse young women with breast cancer
Submit a paper here
Statistical analysis
In this study, the primary objective was to use the MBSR survivorship program to improve the survivors’ outcomes at 12 months compared with baseline using the following measures: PHQ-9 for depression, GAD-7 for anxiety, and SF-36 for QoL using the PCS and MCS. Quantitative data were described using the mean and standard deviation, and categorical data were described using frequency and percentage. The outcome measures were compared between patients who completed 12-month follow-up and those who did not, using unpaired t test. The change in outcome measures at 12 months from baseline was evaluated using paired t test. The effect of intervention was summarized using relative percentage change. The “dose” of the intervention was categorized the number of MBSR sessions – ≤4 sessions, 5-7 sessions, or ≤8 sessions. The change in outcome measures were compared among three groups using 1-way analysis of variance (ANOVA) followed by post hoc multiple comparison using the Bonferroni adjustment. In addition, the effect of intervention on each outcome was evaluated by important baseline characteristics of patients. In each subgroup, the changes were compared with baseline measures using the paired t test, whereas changes in outcome between groups were compared using the unpaired t test. Statistical analyses were conducted using SAS 9.3. P-values less than 5% were considered to be significant.
Results
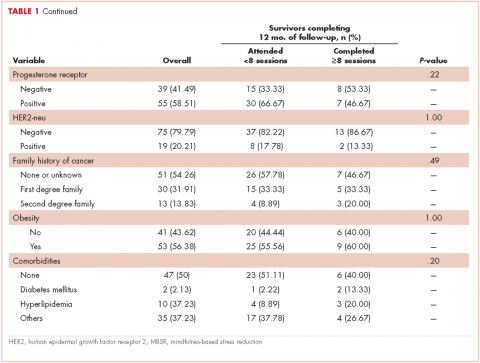
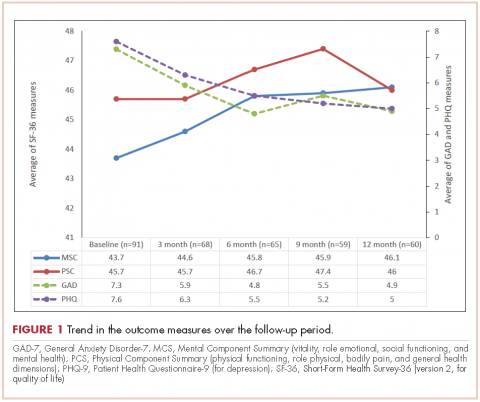
A total of 94 survivors of breast cancer were included in this study and 60 (63.8%) completed the 12 months of follow-up. The average age of the participants was 54.4 years (SD, 8.7), and 90.4% were Hispanic (Table 1). Tumor characteristics were as follows: invasive ductal carcinoma (84.04%), estrogen receptor–positive (ER-, 71.28%), progesterone receptor–positive (PR-, 58.51%), and HER2-neu–positive (20%). In regard to therapy received, 48% of the participants had received anthracycline- and taxane-based adjuvant chemotherapy and 23%, nonanthracycline-based chemotherapy; 71% had received anti-estrogen (hormonal) therapy and 80%, radiation therapy. In regard to surgery, half of the participants had a lumpectomy, and half, a mastectomy. The trends in the outcome measures over the follow-up period are show in the Figure 1.
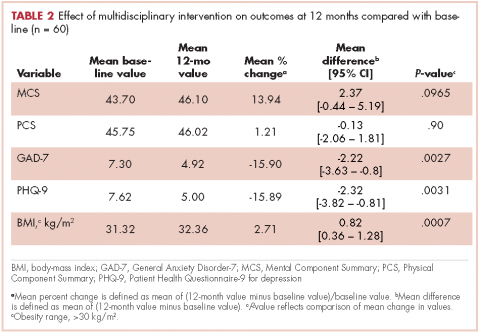
The effect of survivorship program intervention on SF-36 (PCS and MCS), anxiety (GAD-7), and (PHQ-9) at 12 months are shown in Table 2, which also includes the 12-month effects on the body-mass index (BMI). The P-values correspond to the comparison of mean change in scores between baseline and 12-month follow-up. Significant improvement from baseline was observed for PHQ-9 (P = .0031) and GAD-7 (P = .0027). There was a significant trend toward improvement (14%) relative to baseline in the SF-36 MCS at 12 months (P = .097). Although the SF-36 PCS improved numerically, it did not reach to a statistical significance level (P = .896). The BMI at 12 months was found to be statistically significantly increased compared with baseline (P = .0007).
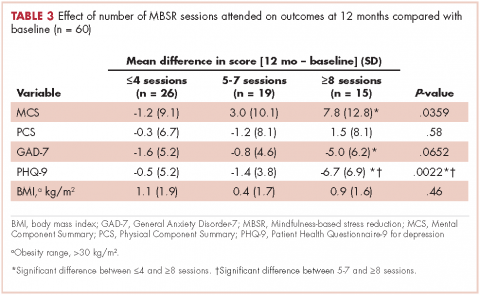
The effect of the number of MBSR sessions attended on the outcome measures is summarized in Table 3. There were significant improvements in the 12-month MCS scores for patients who completed 5-7 sessions of MBSR or ≥8 sessions, compared with patients who completed ≤4 sessions of MBSR. There was an improvement observed in PCS scores only among patients who received at least 8 sessions of MBSR. There was a marked improvement observed in GAD-7 and PHQ-9 among patients who received ≥8 sessions. There was no statistically significant change in the GAD-7 or PHQ-9 scores between patients who received ≤4 sessions and 5-7 sessions. No significant association was obtained between number of MBSR sessions attended and BMI.
The effect of survivorship program intervention on all outcomes according to important baseline cofactors is shown in Table 4. As such, there were no significant differences in changes in the outcome measures after intervention according to any considered baseline characteristics. However, the effect of survivorship program intervention was more pronounced in patients who were ≥3 years away from their initial diagnosis and who had attended a minimum of 80% of the 3-monthly visits and received a minimum of 8 MBSR sessions.
The mean baseline PCS and MCS scores of the SF-36 were 43.7 and 45.8, respectively, indicating that the participants’ scores were significantly less than half the standard deviation below the US norm (50.0; SD, 10). The SF-36 health-related QoL categories showed that, on an average, scores improved by more than 4 units for emotional and physical role functions, vitality, and mental health compared with baseline. In addition, scores improved by about 2 units for general health and social functioning compared with baseline data. In all, 65% of survivors had difficulty preforming work at baseline, but that dropped to 55% after enrollment in the program; and 60% had originally reduced the amount of time spent on work, but that increased to 50% after the intervention. Also of note is that 70% of survivors reported accomplishing less than they would like to have (role physical) before the intervention, but that was reduced to 57% after the intervention. Similarly, 77% of survivors felt worn out at baseline, compared with 65% at the 12-month follow-up; and 88% felt tired at baseline, but that percentage was reduced to 68% after the intervention. Before the intervention, 60% of the participants reported that they had been very nervous, and 45% said they had been so down in the dumps that nothing could cheer them up, but those percentages were reduced to 43% and 32%, respectively, after intervention. Before intervention, 63% of the women said they felt depressed and that was reduced to 50% after the intervention.