Data Trends 2025: Dermatology





Reviewed by:
Brett Sloan, MD, Professor of Dermatology, University of Connecticut School of Medicine; Residency Program Director, Department of Dermatology, University of Connecticut Health Center, Farmington, Connecticut. Brett Sloan, MD, has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: University of Connecticut; Department of Veterans Affairs Received income in an amount equal to or greater than $250 from: University of Connecticut; Department of Veterans Affairs.





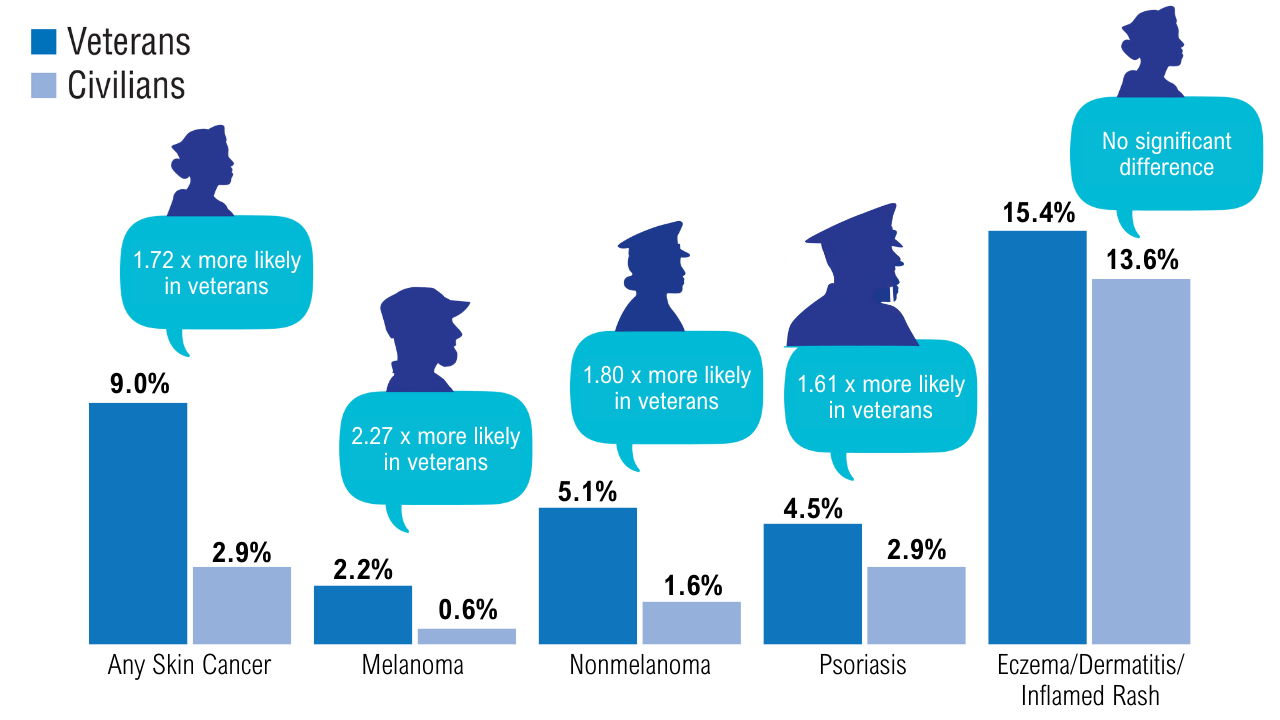
Service members experience unique risk factors for dermatologic conditions, such as increased sun exposure, crowded living conditions, environmental contaminants, skin injury, and extreme temperatures.1,2 Veterans have an estimated 72% higher risk for any skin cancer compared to civilians, and are also at an increased risk of psoriasis, a chronic immune-mediated skin condition.1,3 Dermatitis and eczema are also common conditions in military personnel, accounting for 17.0%-38.7% of skin diagnoses during military missions in Lebanon, Iraq, and Sudan.2
 Prevalence of Dermatologic Conditions in Veterans1
Prevalence of Dermatologic Conditions in Veterans1
This study of approximately 7000 veterans and more than 50,000 civilians, analyzing data from 1999-2018, found that veterans had a higher prevalence and increased odds of skin cancers and psoriasis, but not eczema/dermatitis/rashes compared with civilians. Veterans were 22% more likely to be outside during a workday and had a 44%-45% increased risk of severe sunburn after 30 minutes of exposure.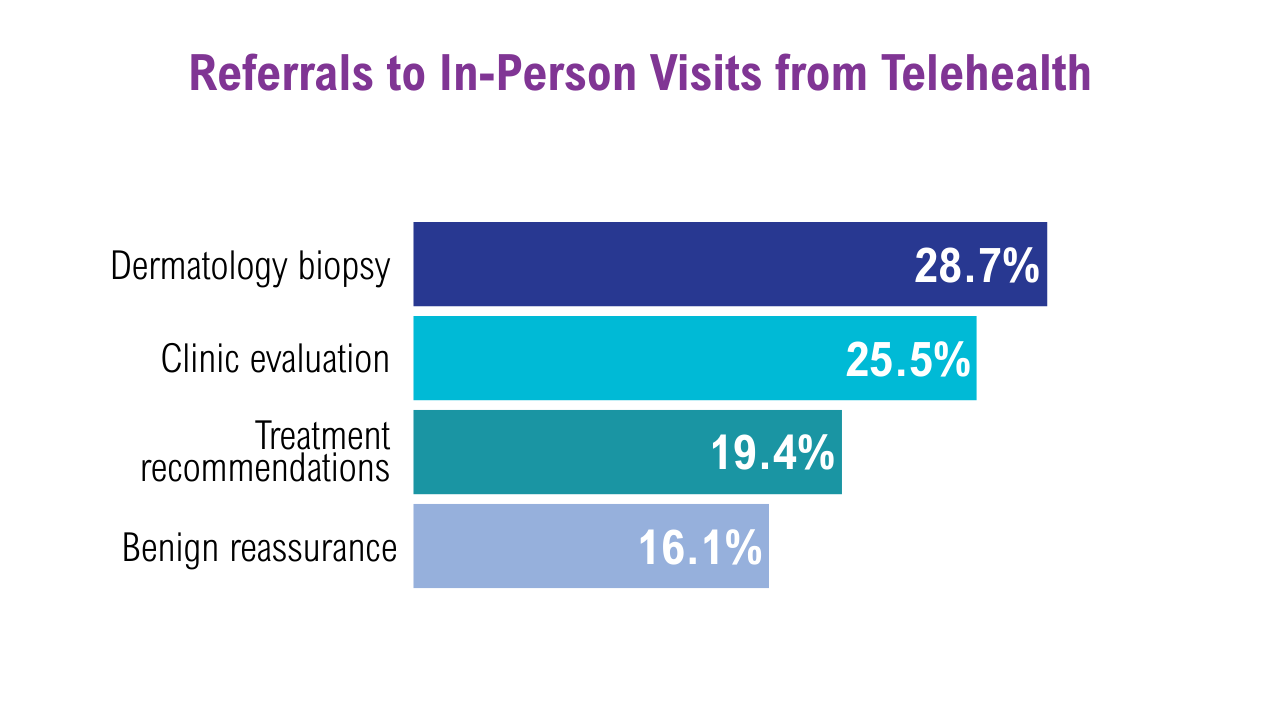 Teledermatology in the VA4
Teledermatology in the VA4
A recent retrospective study of nearly 4500 patients from VA sites across Tennessee and Kentucky looked at trends in teledermatology use from May 2017 through August 2019.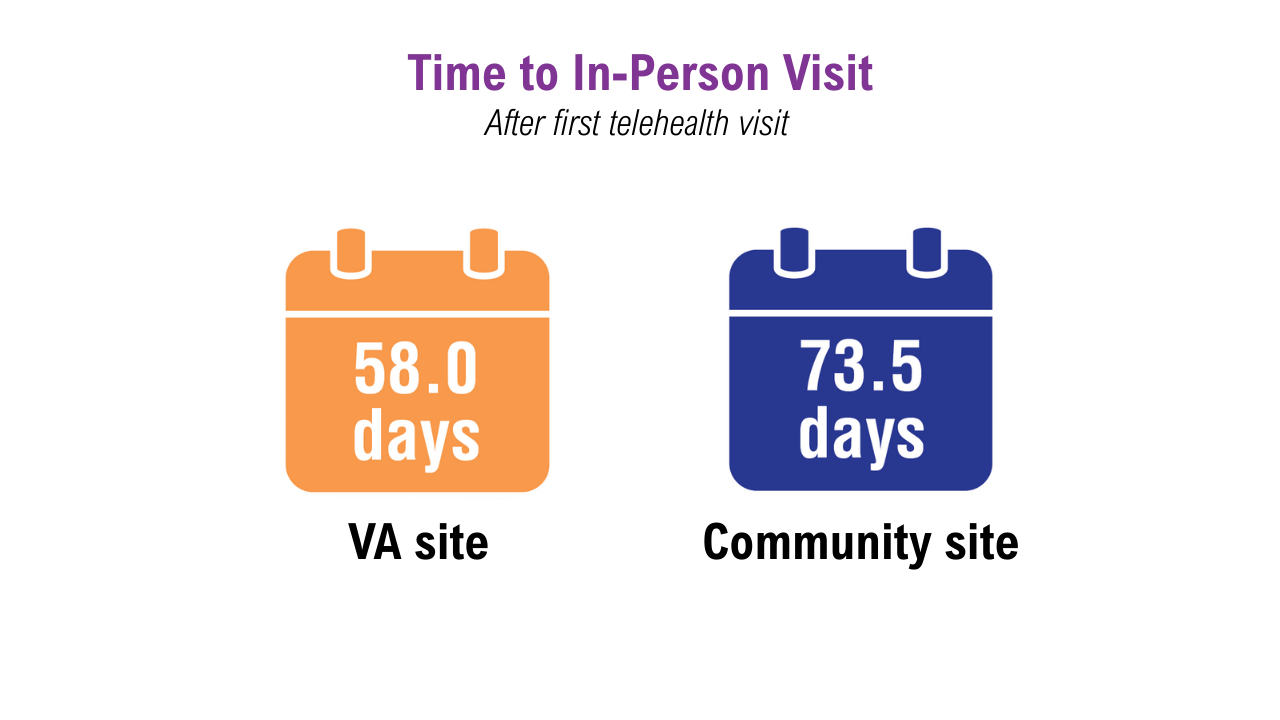 Teledermatology in the VA4
Teledermatology in the VA4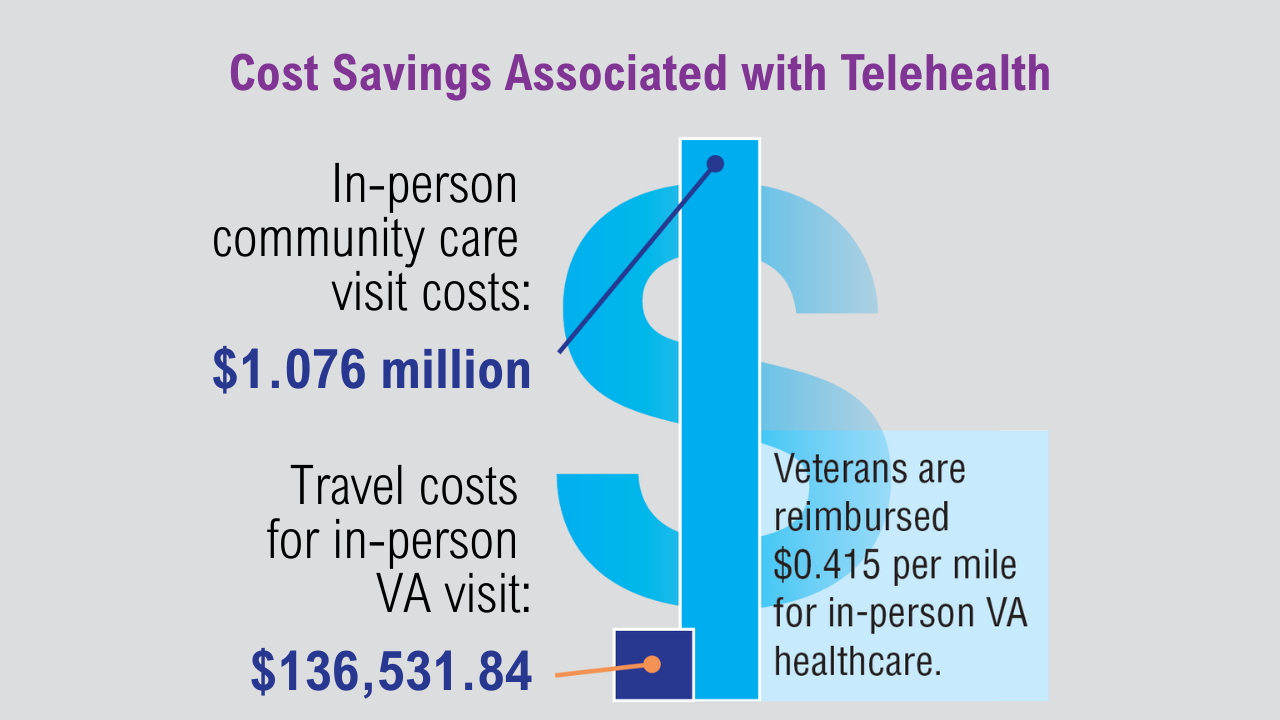 Teledermatology in the VA4
Teledermatology in the VA4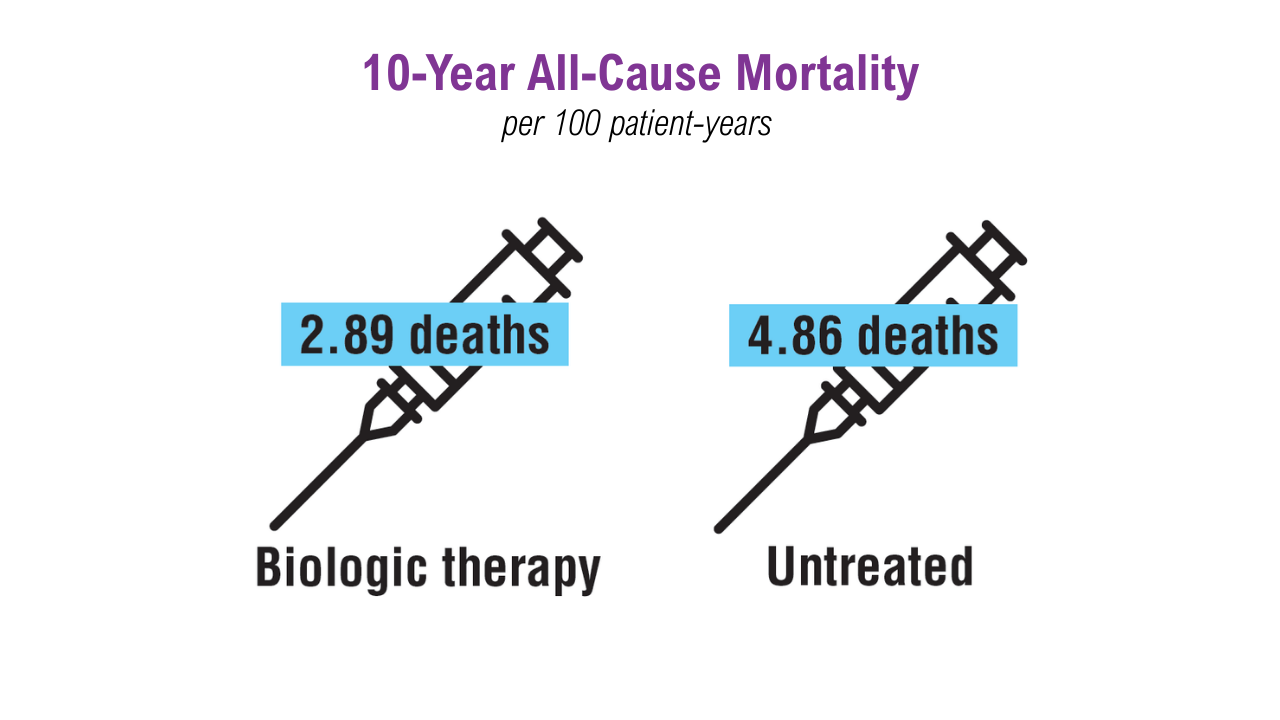 Treatment Mortality Trends in Patients with Psoriasis3,5,6
Treatment Mortality Trends in Patients with Psoriasis3,5,6
Plaque psoriasis may worsen during deployment due to stress, temperature extremes, insect bites, and skin injuries. Poor control can interfere with wearing protective gear and may disqualify individuals from service. A VA study of 4357 with psoriasis patients examined mortality rates by treatment type: biologics, nonbiologics, or no treatment.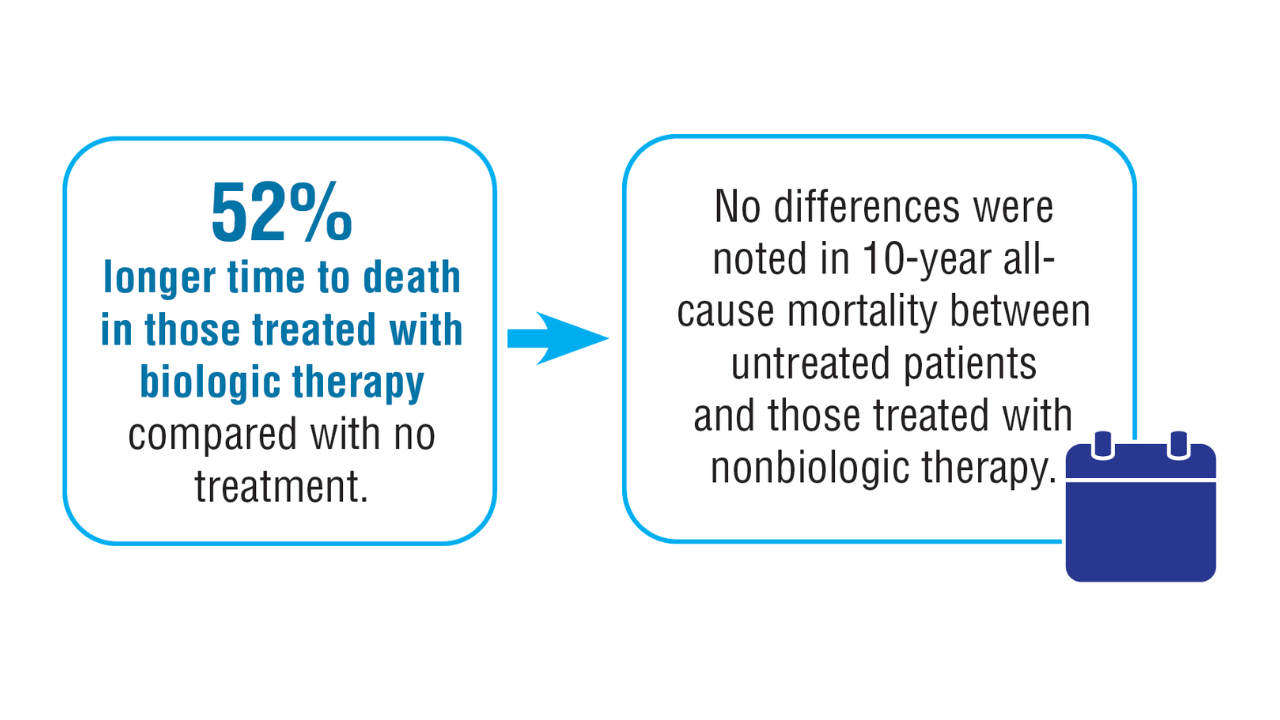 Treatment Mortality Trends in Patients with Psoriasis3,5,6
Treatment Mortality Trends in Patients with Psoriasis3,5,6
Patients on biologics had decreased 1-year all-cause mortality, although there was no difference in MACE. Previous data have suggested a potential cardiovascular benefit from anti-inflammatory therapy in patients with psoriasis.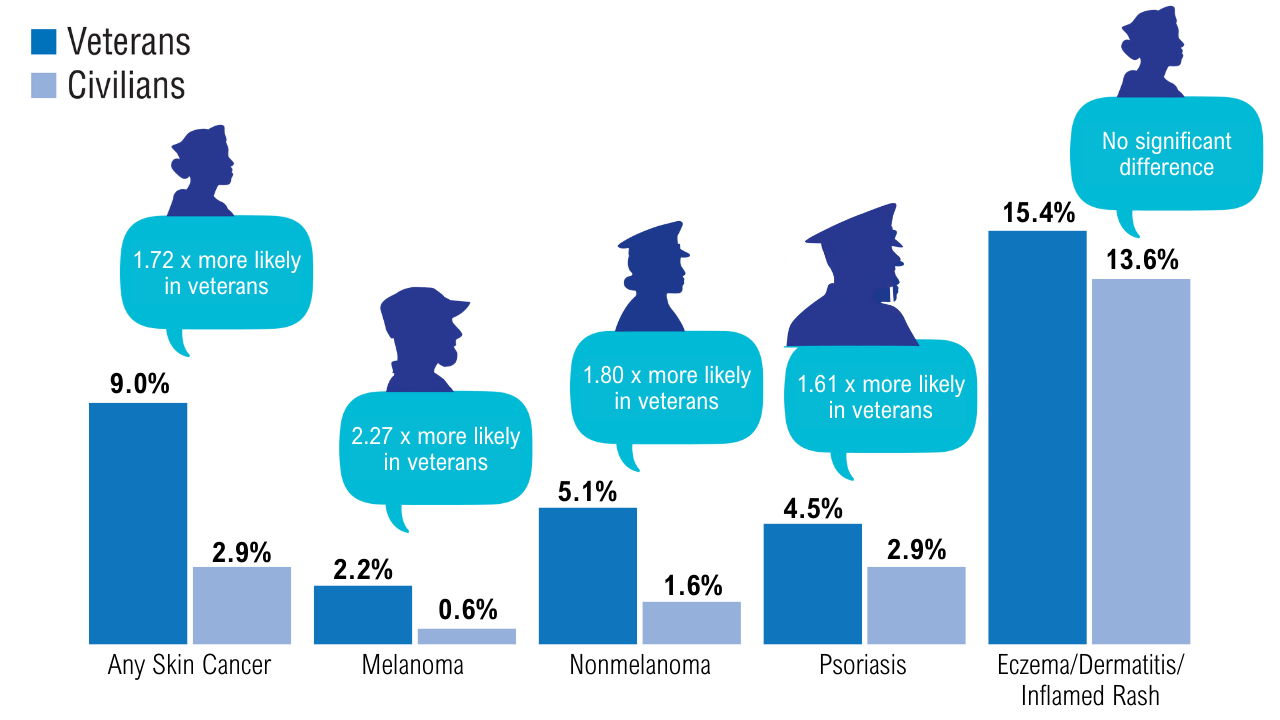 Prevalence of Dermatologic Conditions in Veterans1
Prevalence of Dermatologic Conditions in Veterans1
This study of approximately 7000 veterans and more than 50,000 civilians, analyzing data from 1999-2018, found that veterans had a higher prevalence and increased odds of skin cancers and psoriasis, but not eczema/dermatitis/rashes compared with civilians. Veterans were 22% more likely to be outside during a workday and had a 44%-45% increased risk of severe sunburn after 30 minutes of exposure.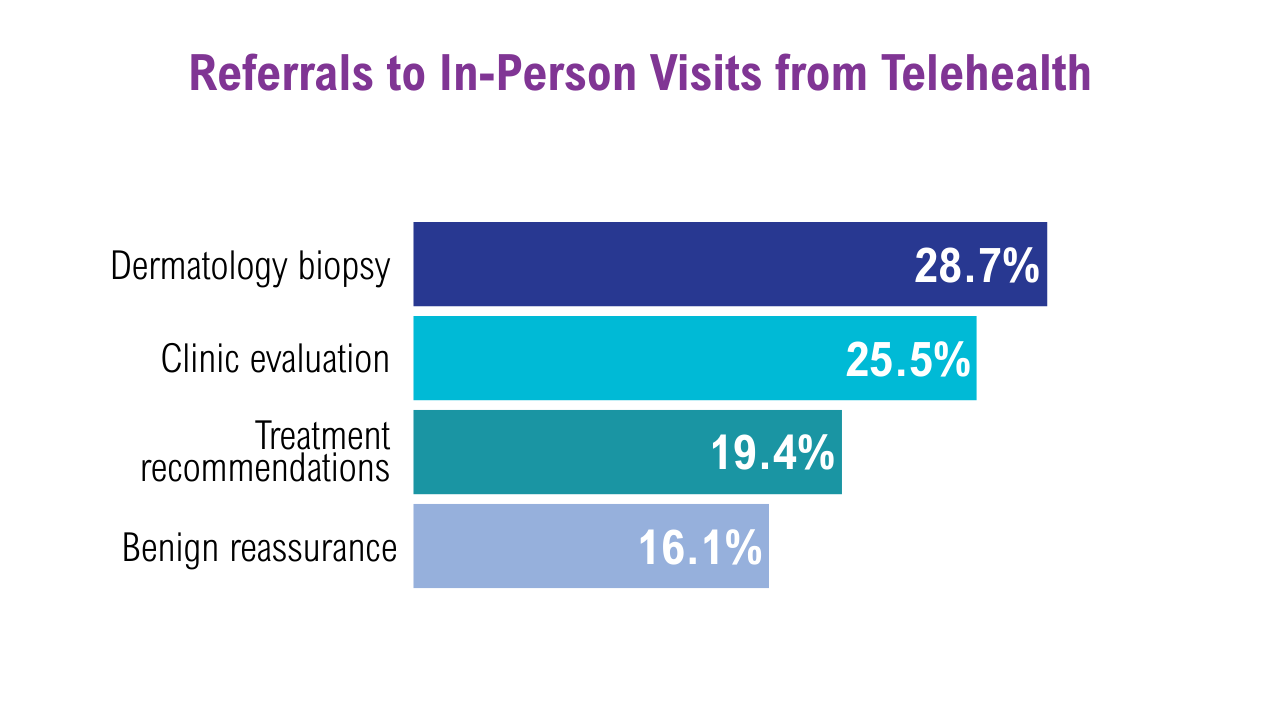 Teledermatology in the VA4
Teledermatology in the VA4
A recent retrospective study of nearly 4500 patients from VA sites across Tennessee and Kentucky looked at trends in teledermatology use from May 2017 through August 2019.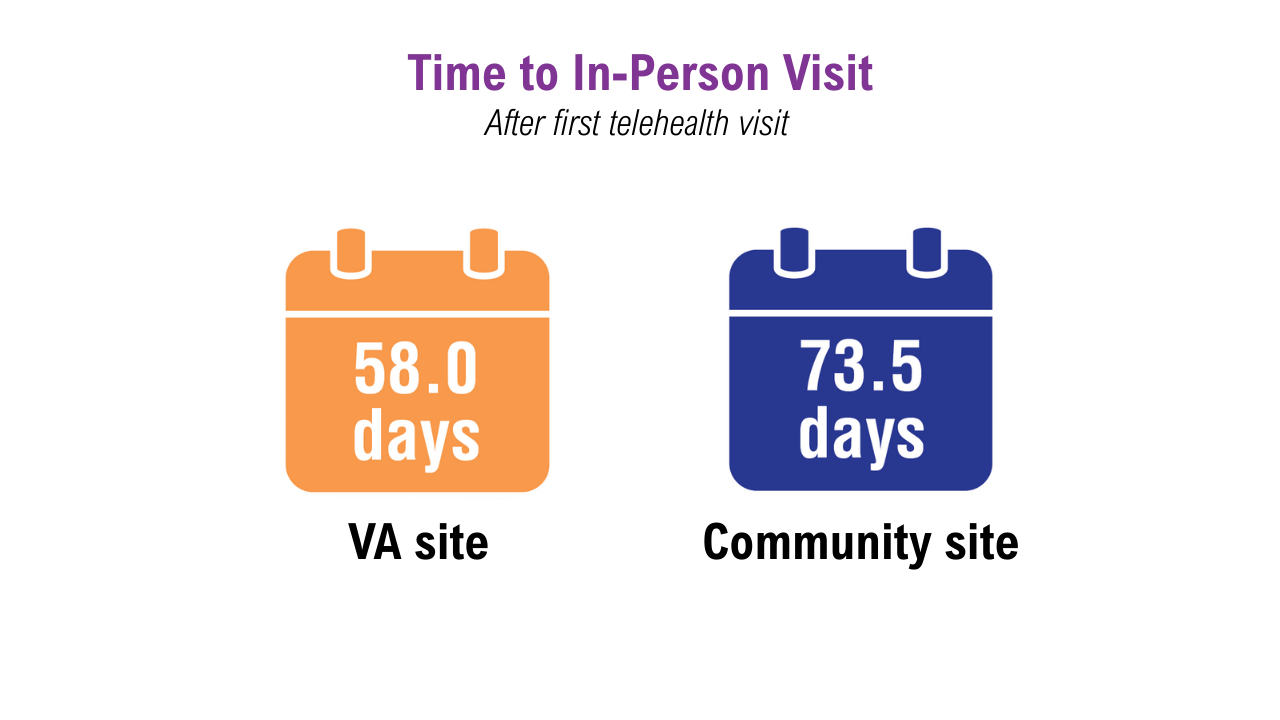 Teledermatology in the VA4
Teledermatology in the VA4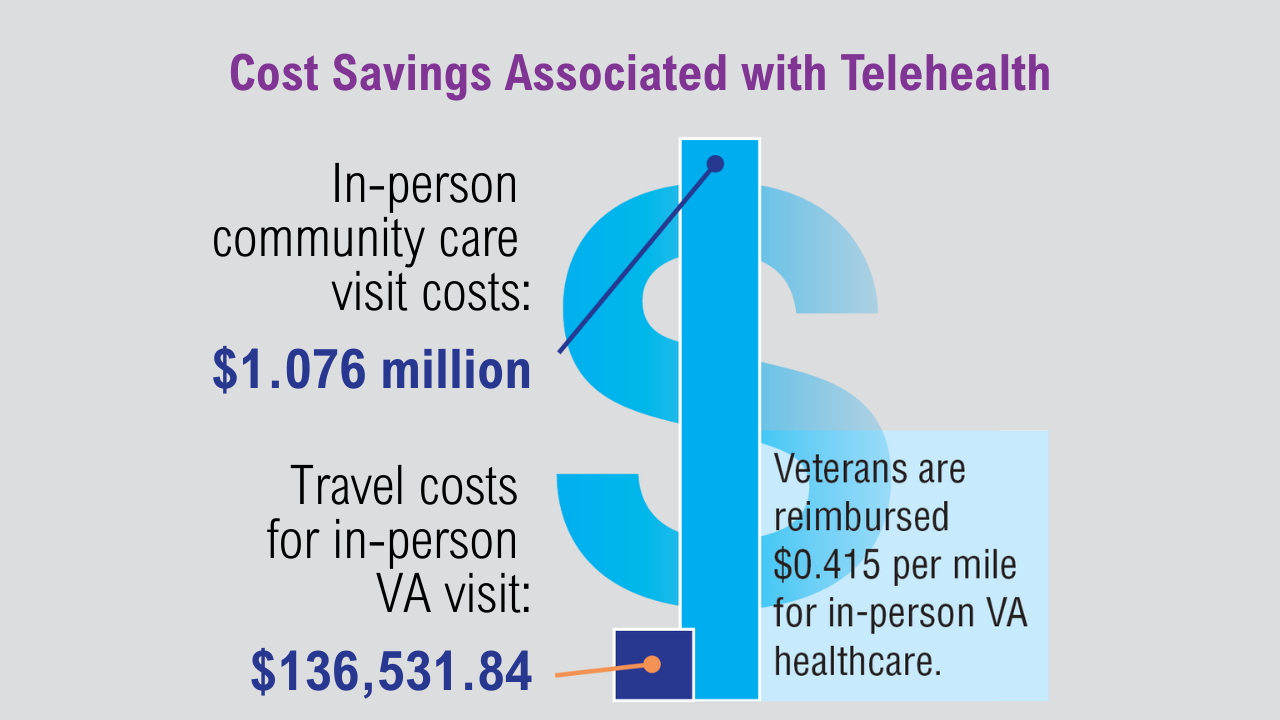 Teledermatology in the VA4
Teledermatology in the VA4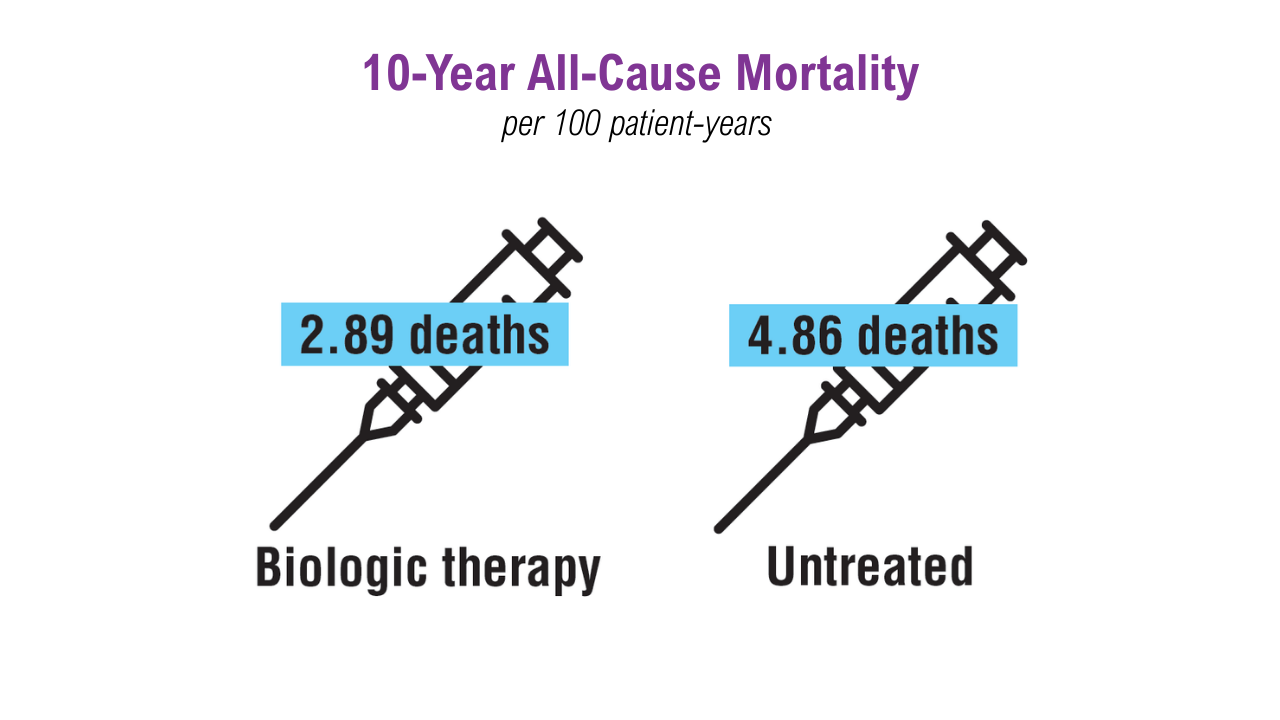 Treatment Mortality Trends in Patients with Psoriasis3,5,6
Treatment Mortality Trends in Patients with Psoriasis3,5,6
Plaque psoriasis may worsen during deployment due to stress, temperature extremes, insect bites, and skin injuries. Poor control can interfere with wearing protective gear and may disqualify individuals from service. A VA study of 4357 with psoriasis patients examined mortality rates by treatment type: biologics, nonbiologics, or no treatment.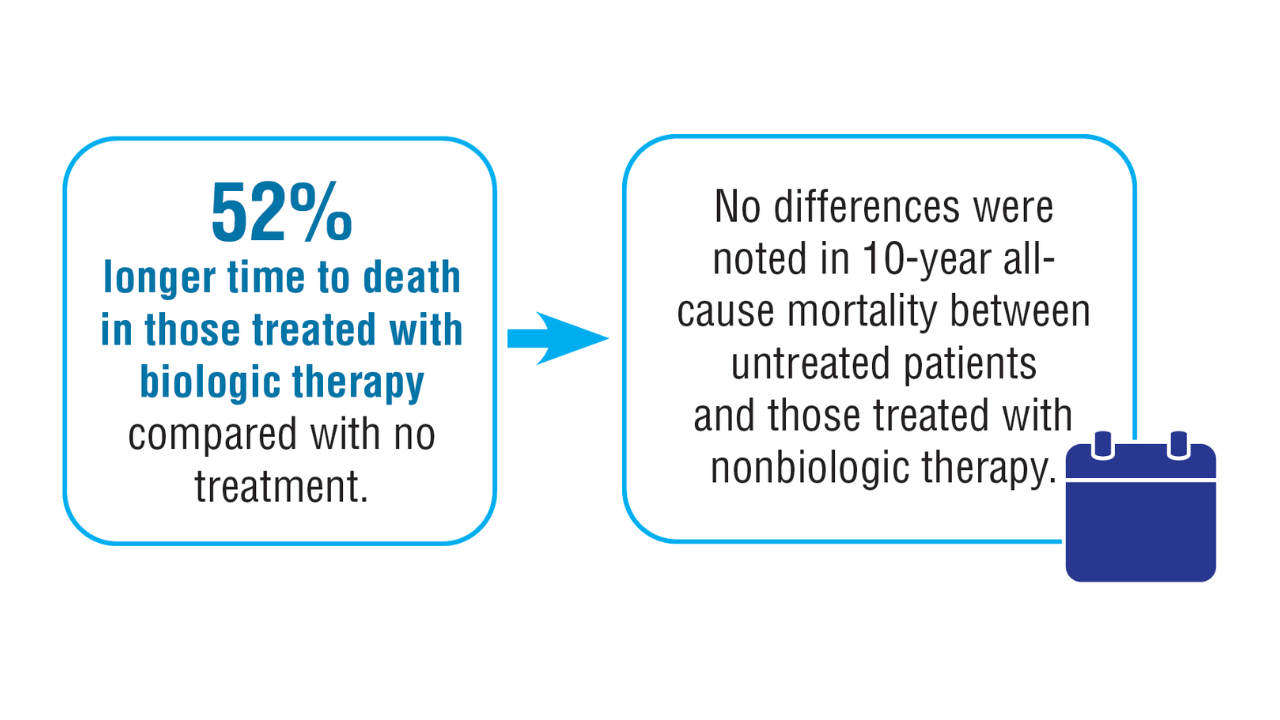 Treatment Mortality Trends in Patients with Psoriasis3,5,6
Treatment Mortality Trends in Patients with Psoriasis3,5,6
Patients on biologics had decreased 1-year all-cause mortality, although there was no difference in MACE. Previous data have suggested a potential cardiovascular benefit from anti-inflammatory therapy in patients with psoriasis.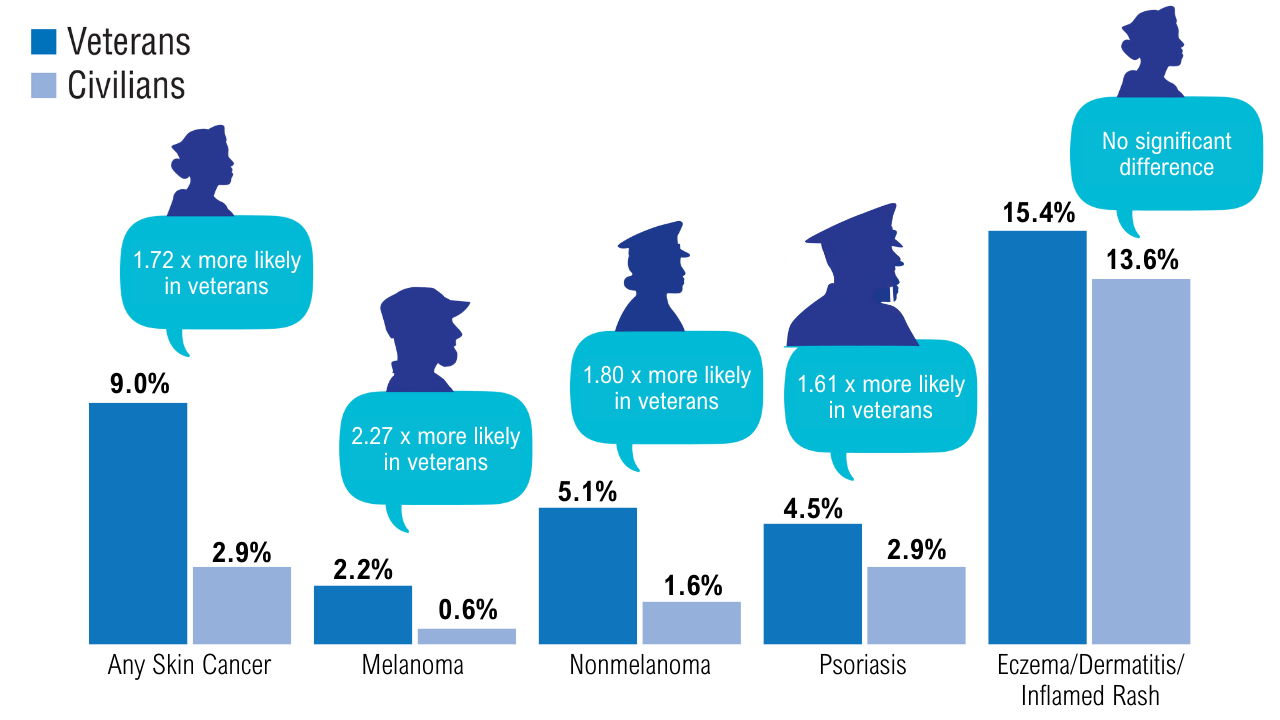 Prevalence of Dermatologic Conditions in Veterans1
Prevalence of Dermatologic Conditions in Veterans1
This study of approximately 7000 veterans and more than 50,000 civilians, analyzing data from 1999-2018, found that veterans had a higher prevalence and increased odds of skin cancers and psoriasis, but not eczema/dermatitis/rashes compared with civilians. Veterans were 22% more likely to be outside during a workday and had a 44%-45% increased risk of severe sunburn after 30 minutes of exposure.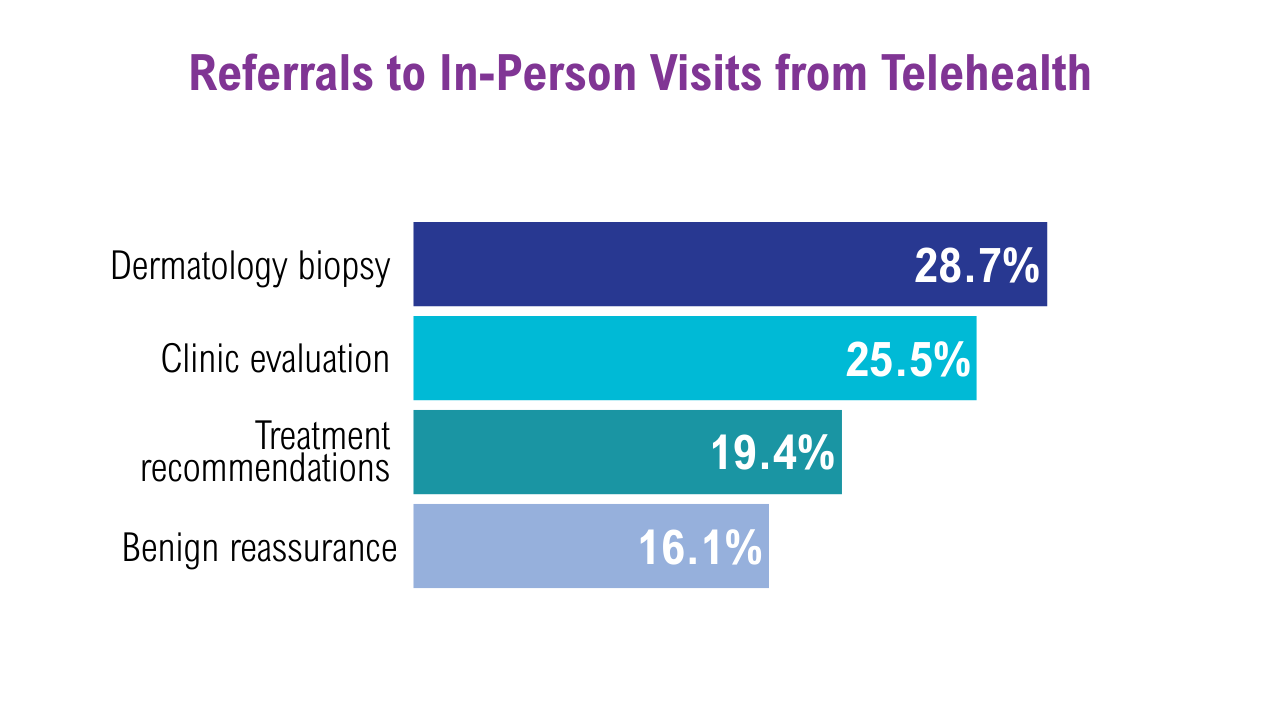 Teledermatology in the VA4
Teledermatology in the VA4
A recent retrospective study of nearly 4500 patients from VA sites across Tennessee and Kentucky looked at trends in teledermatology use from May 2017 through August 2019.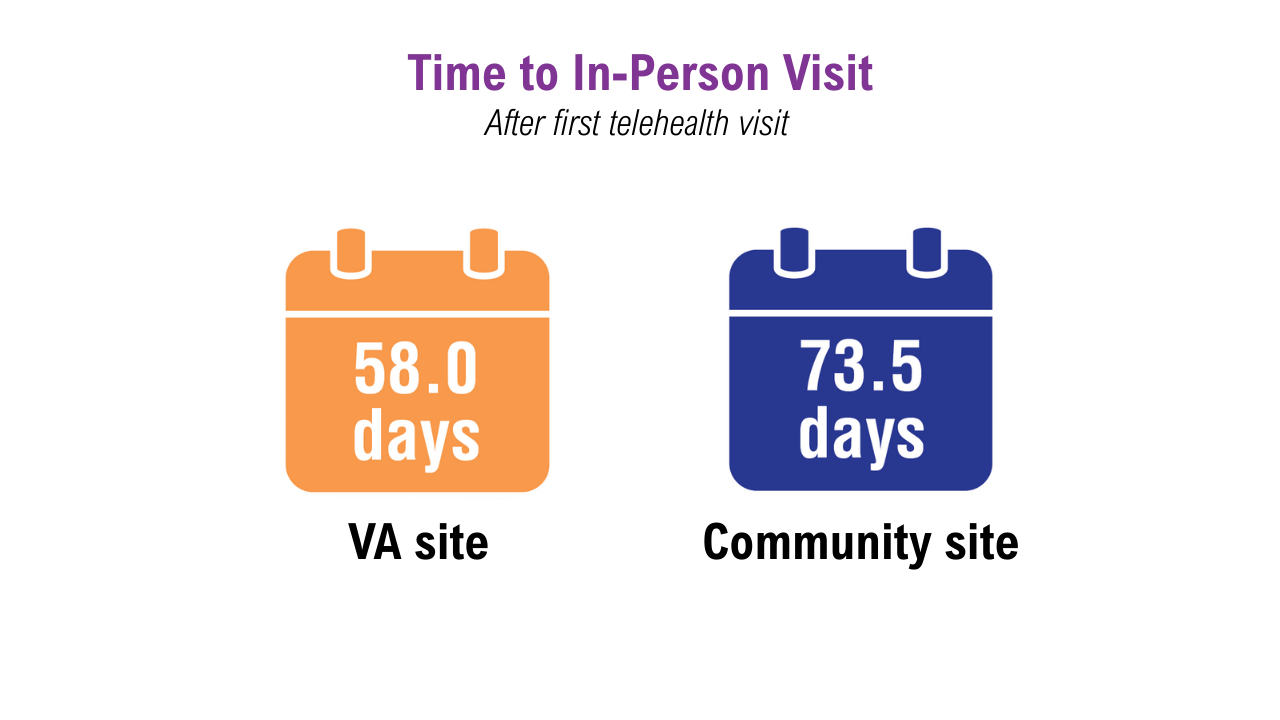 Teledermatology in the VA4
Teledermatology in the VA4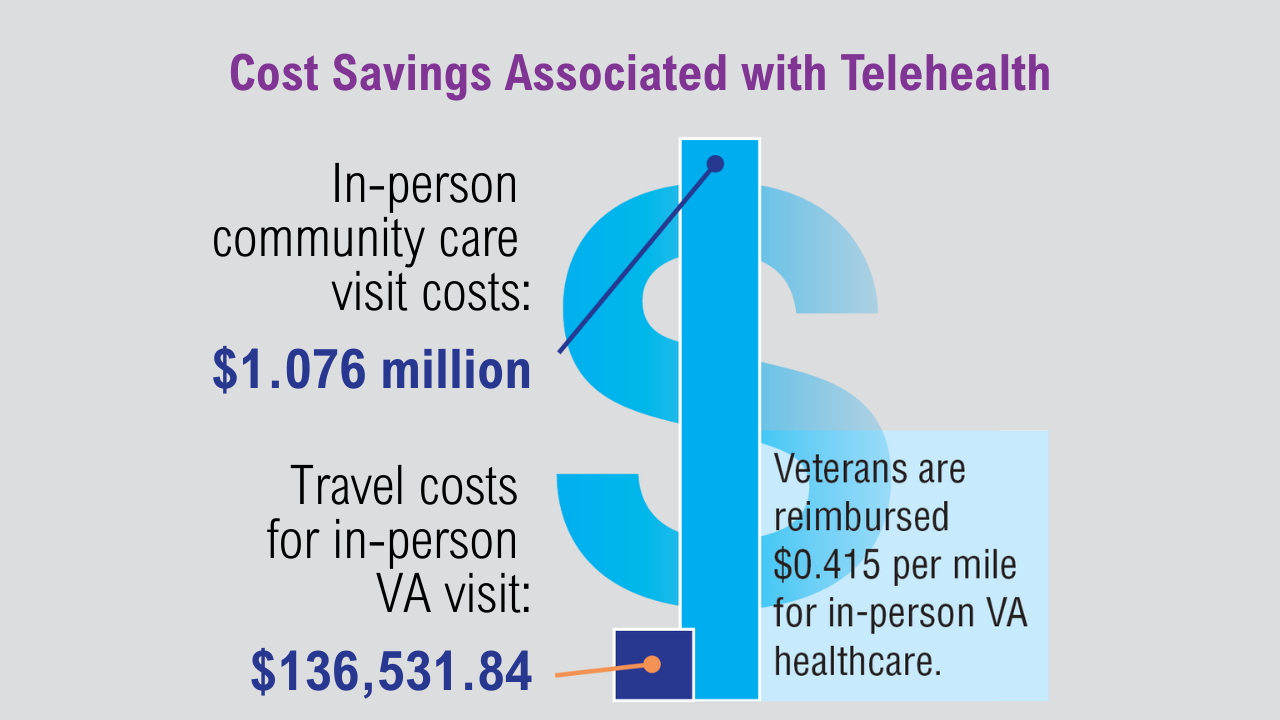 Teledermatology in the VA4
Teledermatology in the VA4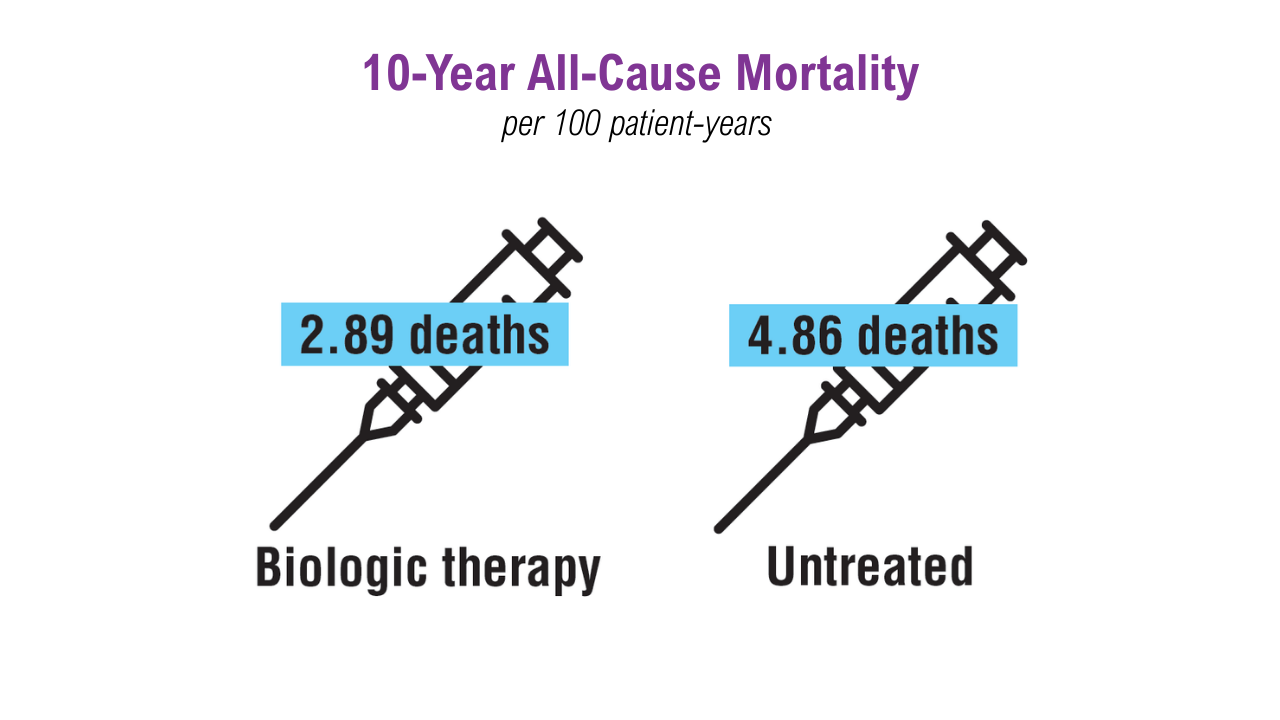 Treatment Mortality Trends in Patients with Psoriasis3,5,6
Treatment Mortality Trends in Patients with Psoriasis3,5,6
Plaque psoriasis may worsen during deployment due to stress, temperature extremes, insect bites, and skin injuries. Poor control can interfere with wearing protective gear and may disqualify individuals from service. A VA study of 4357 with psoriasis patients examined mortality rates by treatment type: biologics, nonbiologics, or no treatment.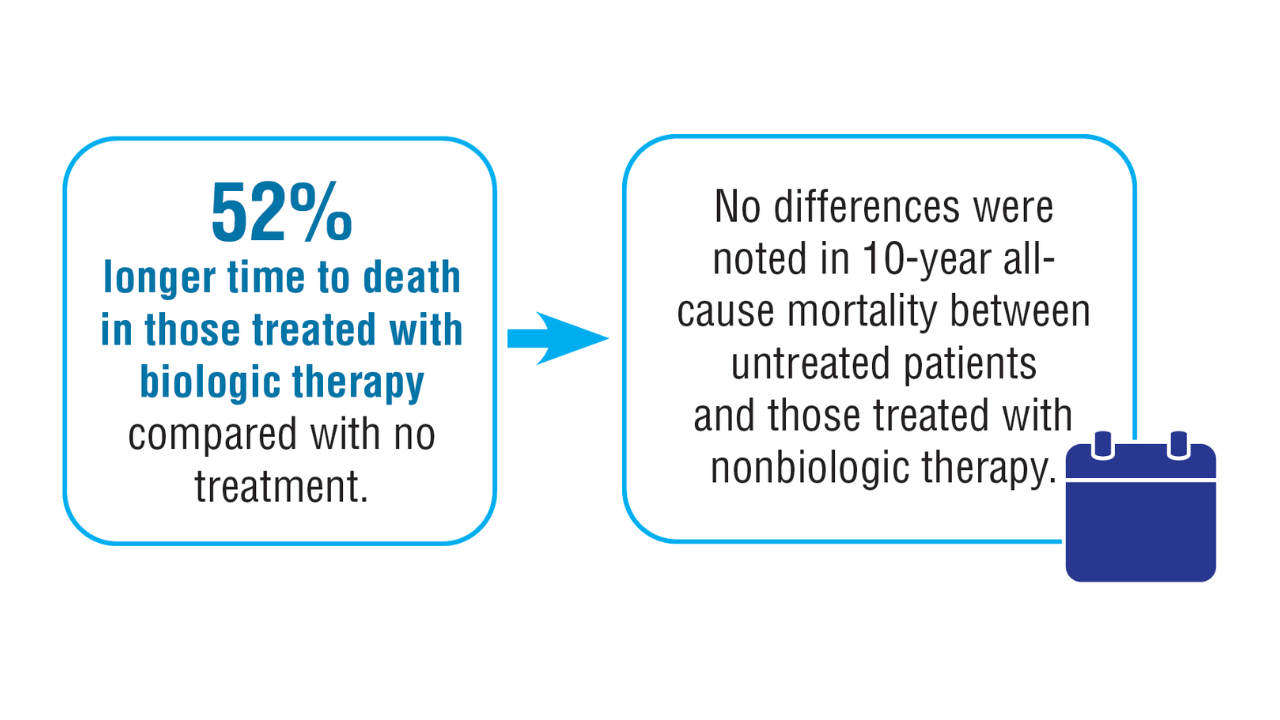 Treatment Mortality Trends in Patients with Psoriasis3,5,6
Treatment Mortality Trends in Patients with Psoriasis3,5,6
Patients on biologics had decreased 1-year all-cause mortality, although there was no difference in MACE. Previous data have suggested a potential cardiovascular benefit from anti-inflammatory therapy in patients with psoriasis.
Click here to view more from Federal Health Care Data Trends 2025.
,false