Understanding and Treating Balance Impairment in Multiple Sclerosis
From the Department of Rehabilitation and Movement Science, University of Vermont, Burlington, VT.
Abstract
- Objective: To provide insight into the mechanisms and treatment options associated with balance impairments in individuals with multiple sclerosis (MS).
- Methods: Systematic reviews, randomized controlled trials, and noncontrolled studies were examined to collect current data regarding treatment options aimed at improving balance in MS.
- Results: Balance deficits are common in individuals with MS and result from a diverse set of constraints across multiple systems of postural control. Poor balance often leads to increased fall risk, reduced physical activity, added comorbidities, and decreased quality of life. A variety of exercise options are available for individuals with MS who experience balance and mobility problems. Physical interventions include targeted therapies, such as vestibular rehabilitation and weighted torso training, as well as more general exercise and balance training prescriptions.
- Conclusion: The evidence, albeit preliminary, suggests that therapeutic intervention aimed at ameliorating balance deficits associated with MS be multimodal. Exercise prescriptions should include sensory and motor strategy training, strength development, as well as functional gait activities. Further evidence-based research is needed to improve the management of balance deficits in those with MS and to identify the impact of improved balance on activity participation and quality of life.
Multiple sclerosis (MS) is one of the most common nontraumatic neurologic causes of disability among young adults. With greater awareness and improved diagnostics, more people are being diagnosed with the disease today than in the past. Prevalence estimates in the United States range from 90 to 135 per 100,000 individuals [1], with approximately 400,000 people currently diagnosed [2,3].
MS is a chronic inflammatory disease of the central nervous system typically characterized by increasing muscle weakness, spasticity, fatigue, pain, depression, visual and sensory disturbances, and cognitive difficulties. The clinical course of MS is highly variable and often unpredictable with increasing disability and physical decline spanning a 30- to 40-year period post diagnosis [4]. During this time, advancing symptoms can lead to a number of comorbidities and negatively impact daily functioning, mobility, and community participation [5–7]. From a public health standpoint, the early and disabling impact of symptoms and prolonged physical decline create a significant economic burden. The projected national heath care costs of MS are greater than $7 billion annually [8], with the average total annual cost per patient estimated at over $47,000 [9]. Of this annual cost, indirect costs associated with lost productivity represent the single highest component cost [9,10].
Of the wide range of disease-related challenges, mobility difficulties are most significant. Over 90% of people with MS report mobility difficulties [11], and maintaining mobility is consistently ranked as one of the highest priorities for this group, independent of disease duration or disability level [10,12]. Several studies have demonstrated that loss of balance and mobility contributes to substantial patient burden [13] and lower perceived quality of life [10]. Moreover, poor balance and increased fall risk have been associated with reduced physical activity and other health-related behaviors [14,15].
Because balance and mobility limitations are so prevalent and impacting, targeted treatments aimed at maintaining ambulation and function are critical goals in the management of MS. It is important for physicians and rehabilitation professionals to understand and recognize the underlying sensorimotor mechanisms related to postural instability and initiate appropriate evidenced-based treatments that can improve balance, reduce fall risk, and enhance quality of life for individuals with MS. This review seeks to analyze the evidence on the physical interventions aimed at ameliorating balance and mobility impairments associated with MS in the context of a case example.
Case Study
Initital Presentation and History
Ms. D is a 41-year-old woman with relapse-remitting MS. She was diagnosed 6 years ago after experiencing initial symptoms of optic neuritis and some numbness in her right hand. Since then, she has developed greater weakness in both her legs and reports that her MS significantly impacts her ability to walk, both in terms of distance and the effort needed to ambulate.
Ms. D is independently ambulatory without the use of any assistive device. She reports that her balance is worse when walking on uneven surfaces, moving about in dimly lit environments, turning, or when walking in crowded spaces. Ms. D also shares that she has difficulty standing on one leg while pulling on socks. She states that she must concentrate and focus on her balance when in these challenging situations and that she has to consistently look where she is stepping.
Ms. D does not have any spasticity in muscles of the lower extremities, but on occasion does experience some numbness and tingling in her left foot. She experiences moderate fatigue that requires her to pace herself throughout her daily activities. She reports that her fatigue impacts her ability to concentrate or pay attention for long periods of time and impacts her motivation to engage in social activities. She states that she sleeps restlessly and is consequently tired when she wakes in the morning. Although she is sedentary, she has no history of cardiopulmonary issues or orthopedic problems.
Physical Examination
Ms. D is 5’7” and weighs 175 pounds, with a BMI of 27.4. She presents with observable gait and balance impairment. On physical examination, she exhibits reduced bilateral strength of knee flexors and extensors as well as hip adductors, although the weakness is more evident on the left. On neurologic exam, she exhibits moderate disability in both sensory and cerebellar functioning (resulting in an Expanded Disability Status Scale score of 3.5) [16].
What is postural control?
What balance impairments are associated with MS?
Postural Equilibrium and Balance
For all individuals, postural orientation and equilibrium underlie the effective performance of life’s daily tasks. Postural orientation refers to the alignment of body segments to a reference (such as gravity, the support surface, or an object in the visual field), while postural equilibrium—often equated with balance—refers to maintaining or re-acquiring the body’s center of gravity (CoG) within the base of support (BoS) [17,18]. This paper will focus on postural equilibrium with MS across multiple contexts of balance tasks.
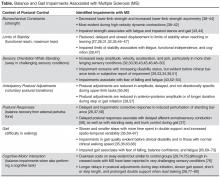
Horak [18] described contexts of balance tasks that affect the mechanisms of maintaining postural equilibrium. Some of these contextual variables include
- Biomechanical constraints (eg, strength)
- Limits of stability (functional reach, maximum lean)
- Anticipatory postural adjustments (voluntary postural transitions)
- Automatic postural responses (balance recovery from external perturbations)
- Sensory orientation (ability to reweight sensory information [somatosensory, visual, vestibular] depending on context
- Dynamic control during gait
- Cognitive-motor interaction (balance impairments when also performing a cognitive task)
Emotion represents another contextual variable of interest, because mood and fear can significantly modify postural control [19–23]. Knowing the contextual factors that modify balance control provides insight into underlying neuropathology associated with impairments of these postural control variables [24,25] as well as insight into what should be included during the examination of patients with MS based on patient descriptions of their symptoms and functional challenges.
Balance Assessment
Balance assessment indicates that Ms. D cannot abduct and hold either leg to her side for any noticeable length of time, cannot reach forward adequately without lifting her heels off the ground or falling forward, and cannot stand on one leg for more than 10 seconds without losing balance. She also needs to take multiple steps to recover balance with any slight perturbation and is unable to maintain stability while standing on foam with her eyes closed. She shows significant imbalance when rising from a chair, walking forward, and turning to come back to sit.
For Ms. D, the clinical balance exam suggests pervasive impairment of hip strength, limits of stability, anticipatory postural adjustments, postural responses, sensory integration, and gait. Furthermore, her reported need to focus vision on her gait is in accordance with compensation for existing sensory impairments. Lastly, fatigue and attention demand likely enhance the presentation of balance impairment.
What are the consequences of balance impairments associated with MS?
Balance impairments present considerable health problems for adults with MS. Greater than 50% of individuals with MS report falling in any 6-month period [81–85], with the incidence of recurrent falls reported to be as high as 9 falls per year [86]. In addition, fall-related injuries, including fractures, are more common with MS, although this increased risk is considerably greater for women with MS than men [86–90].
Common risk factors for falling in people with MS include variable or deteriorating MS status [90–96], problems with balance or mobility [88,92–94,96–99], use of walking aids [88,93,97], lower balance confidence [86,98], reduced executive functioning [99] and greater fatigue [85]. Increased postural sway [52,99,100], slower walking speed [99], greater gait asymmetry and variability [92,101], slower choice stepping reaction time [99], impaired forward limits of stability [92,99], impaired visually dependent sway [92,99], and leg weakness [88,92] have also been found predictive of future falls in MS. A link has also emerged between cognitive impairment and fall risk [86,95,99,102].
Fear of falling and fall-induced injuries are also the most common causes of restricted activity and disability for individuals with MS [14]. Research has shown that future physical activity associates with fear of falling, and fear of falling subsequently associated with lower-limb strength asymmetry and decreased limits of stability rather than past experience of falling [103]. Similarly, the perceived benefits of physical activity and an individual’s self-efficacy to engage in physical activity predict reported levels of physical activity independent of disability level for individuals with MS [104]. Thus, psychological perception represents an important, and potentially modifiable, correlate of physical activity.
Moreover, individuals with MS experience a high risk of cardiovascular disease and other chronic health conditions associated with deconditioning, as unfavorable blood lipid levels, poor glucose profiles, and obesity have been observed in this population [105]. Comorbid conditions, secondary conditions, and health behaviors are increasingly recognized to be important factors influencing a range of outcomes in MS [107].
Further History
Consistent with the consequences of balance and mobility impairment, Ms. D reports that she loses her balance and nearly falls at least 1 time per week while engaged in daily activities. She also shares that she fell 2 months ago while walking outside and across the lawn to get the mail. Her confidence is low for many daily tasks such as climbing stairs, picking up objects from the floor, reaching when on tiptoes, or walking on ramps or on slippery surfaces. While Ms. D is independent in all activities of daily living, she currently does not work due to her fatigue and poor balance. She indicates that she is not very physically active and feels somewhat isolated and depressed because her balance and mobility challenges keep her from going out with friends and socializing.
What exercise approaches are available to ameliorate the balance deficits associated with MS?
There are a variety of therapeutic approaches for the treatment of poor balance in MS. While pharmacologic treatment typically encompasses disease-modifying therapies, specific medications can also help in the management of symptoms (ie, fatigue, spasticity, gait variability) that can negatively impact balance and mobility. Other rehabilitative strategies for balance impairment include gait training, assistive devices for mobility, and environmental modifications for fall prevention. Although all of these avenues offer viable treatment options for improving balance, exercise is increasingly appreciated as an important adjunct to the rehabilitation management of MS [107], especially in terms of improving balance deficits, optimizing daily functioning, and increasing participation across various life contexts.
The diversity of exercise options available for individuals with MS who experience balance and mobility problems is expanding. Moreover, mounting evidence suggests that exercise is well tolerated by participants with the disease[108–110] and that individuals with MS can exercise sufficiently to improve their fitness, function, and quality of life [109,110]. Given the inherent variability of MS and the heterogeneity of symptoms and disease course across individuals, however, no one exercise prescription is optimal for all those diagnosed. Instead, treatment goals must be individualized and functionally based [107] with ongoing evaluation and modification of treatment plans due to disease progression, symptom fluctuations, and functional decline [107,111]. Regardless of specific approach, the aim of any exercise intervention is to reduce activity limitations, encourage participation, and facilitate independence and life satisfaction in those with the disease [112].
Resistance Training
There have been several structured reviews of exercise research in MS [108,110,113,114]. The existing evidence supports resistance exercise as compared with no exercise for improving general balance [115] or performing tasks such as a chair transfer [116] or sit-to-stand [117]. Two randomized controlled trials (RCTs) also revealed significant increases in functional reach (ie, limits of stability) as a result of progressive resistance exercise [118,119]. Resistance exercise has not, however, facilitated greater benefit over traditional rehabilitation in other postural control contexts such as those involving postural transitions, sensory integration, or postural sway [120–122].
The effects of resistance training on mobility have also been inconsistent. While several studies showed no significant improvement in functional mobility [118,122,123], a positive improvement was observed in other research [119,124,125]. Likewise, stair climbing was shown to improve in 2 noncontrolled studies [125,126] and one RCT [117] but not in another [127].
In a recent RCT to evaluate the comparative effectiveness of different methods of resistance training, Hayes et al [123] determined that the addition of high-intensity, eccentric resistance training offered no additional benefit over standard concentric resistance exercise in improving static standing balance and stair climbing. In addition, compared with no exercise or a home-based program to improve strength and balance, progressive resistance cycling showed significantly greater effect on functional reach and timed up-and-go in individuals with moderate MS [128]. Nonetheless, evidence for the efficacy of home-based training remains equivocal given issues of motivation, adherence, and training intensity [115,118,128].
Taken together, the systematic reviews to date conclude that there is insufficient evidence for the effects of resistance exercise on balance in MS, thus making solid evidenced-based conclusions difficult [108,110,113,129]. Moreover, it is difficult to ascertain a definitive and most efficacious exercise prescription for improving balance in MS given the inconsistency in protocols and findings across studies. There is some support, albeit preliminary, for progressive resistance training as a modality to improve balance, especially those functional tasks demanding greater strength [113]. Nonetheless, resistance training may contribute to improved posture and gait given it directly addresses one context of postural control, but it may not be fully effective due to lack of training to modify central neural control of posture in other contexts.
Aerobic Exercise
Many of the studies examining aerobic exercise in MS more often target walking capacity, exercise tolerance, fatigue, and quality of life than balance [130]. The limited research that has focused on aerobic exercise for balance improvement has shown equal benefit to that achieved from resistance exercise in those contexts involving limits of stability and dynamic balance while stepping or walking [119]. This finding was reasonable given that the aerobic exercise included step-up and treadmill walking. Still, it has been recommended that, for most people with MS, aerobic exercise also incorporate a degree of balance training [109].
Combined Exercise
The more recent exercise research involving people with MS often combines some aspect of aerobic, strengthening, and/or balance exercise. While only a few RCTs have examined the effects of combined training in this population, preliminary evidence suggests it is well tolerated and may have some benefit for improving function [110]. While one study found no differences in static balance after a combined strength and aerobic training program [131], review of the exercise protocol revealed that the training regime had only incorporated 2 standing exercises. Other studies more intentionally combining strength and balance exercise have demonstrated benefits in balance confidence [132], standing static balance or postural sway [132–134], step climbing [133], and functional mobility [135]. Combining aerobic exercise and strengthening has also been effective in reducing falls in those with MS [85].
Balance-Specific Exercise
Only one balance-specific RCT has been published to date. In this study, outcomes from balance training involving both motor and sensory strategies were compared to training of only motor strategies and to standard therapy [136]. Both the balance training groups significantly reduced the number of falls post intervention as compared to the conventional treatment group. There were no observed differences in self-reported balance confidence across the groups, although both the balance training groups significantly improved in static and dynamic standing balance over that achieved by the standard treatment group. The fact that only the group engaged in sensory training differed significantly on dynamic gait highlights the importance of sensory integration for dynamic balance and gait.
Video Game–Assisted Exercises
Novel rehabilitative approaches have taken advantage of advances in virtual reality and visual feedback training to improve balance and mobility deficits in people with MS. Exercise using the general physical activity games on the Nintendo Wii Fit provided short-term improvement in standing balance, strength, gait and physical activity in people with MS [137]. This general exercise offered no significant gains in self-efficacy, fatigue impact or quality of life, and physical activity levels returned to baseline levels 14 weeks after exercising. Subsequent review has, however, highlighted concerns that current commercially available video options for general exercise may not be sufficiently adaptive for people with moderate disability, leading to intimidation and low adherence [138].
Beyond general physical activity, the Wii Balance Board System has also been used to specifically target balance and mobility deficits in MS. Although one study found no significant benefit from Wii Fit balance exercise in balance performance and walking ability [139], other studies have shown positive effects in standing sway, static balance, dynamic stepping, walking speed, and MS impact [140–142].
The evidence, albeit preliminary, thus suggests that the Wii Fit may offer a feasible adjunct to traditional rehabilitation approaches, especially because the exercise can be done at home without the need for continuous support from a practitioner and because the technology aids in overcoming access barriers often associated with community-based physical activity programs [138]. Nonetheless, research shows that Wii Balance Board System training is more specific for static standing balance than for dynamic balance or mobility, the technology is not positively viewed by those with more advanced symptoms, and there exists a risk of adverse affects and training-related injuries associated with home-based use of the Wii [137,140].
Vestibular Rehabilitation Exercise
Vestibular rehabilitation is a specialized treatment approach that strengthens the vestibular sensory system by retraining the brain to recognize and process signals from the vestibular system and coordinate these with visual and proprioceptive inputs. To date, there has only been one RCT investigating the effects of vestibular rehabilitation on balance in adults with MS [143]. In this study, the outcomes of a standard vestibular rehabilitation program to those of an exercise regime as well as to no intervention were compared. The vestibular rehabilitation program consisted of static and dynamic tasks performed with changing bases of support, on various surfaces, with eyes open or closed, and different head movements. The 6-week vestibular rehabilitation program resulted in both statistically significant and clinically relevant change in standing balance under various sensory conditions compared with either of the other two groups, although no significant difference was found in walking capacity across groups.
Weighted Torso Training
Balance-based torso weighting (BBTW) involves strategically placing small weights on the trunk of an individual to decrease balance deviations observed during quiet stance, perturbed standing, walking, and transitioning [144]. While the specific mechanism underlying the therapeutic effect of rehabilitative weighting has been debated [145], various suggestions include joint compression to encourage co-contraction, enhanced conscious awareness of body segments, and biomechanical changes via shifting of the center of mass [146].
The one RCT examining the effectiveness of BBTW in people with MS found immediate and significant effects of BBTW on postural control and upright mobility [146]. The research confirmed preliminary investigations of BBTW in MS [144,147], demonstrating that BBTW can improve walking speed as well as functional tasks involving standing, walking, turning, and sitting down.
Whole Body Vibration
Whole body vibration (WBV) has been employed across a variety of neurological populations as a means of improving muscle tone, sensation, strength, stability, and functional performance. In WBV, multidimensional vibrations are transferred to an individual performing static or dynamic movements on an oscillating platform. The vibrations are believed to facilitate both neuroendocrine responses as well as motor unit recruitment [148–150].
Results have been inconsistent regarding the effectiveness of WBV as a way of improving postural control and functional mobility in individuals with MS. A few studies have shown significant positive effects of WBV lasting from 1 to 4 weeks on functional mobility [151–153], strength [151,153,154], walking speed [152,155], and standing balance [152]. Walking endurance has also been affected by vibration training designed to improve muscular endurance [156]. Although there have been noted benefits of WBV, these benefits were not significantly more advantageous than those offered by a vibration program in conjunction with lower-limb stretching and strengthening exercises [157] or in addition to a traditional rehabilitation program [154].
There has also been some evidence to show that prolonged WBV does not improve postural stability or functional mobility in individuals with MS after training [155,156,158]. Likewise, there is contradictory evidence supporting the use of WBV in improving walking speed [157], functional reaching [152,153] or overall quality of life [152].
While WBV does not appear to have a detrimental effect on symptoms of MS, there is insufficient evidence regarding its beneficial effects on balance, gait, muscle strength and quality of life compared to other interventions. Future research is necessary to examine various protocols in terms of vibratory parameters and length of intervention before specific prescriptions can be offered [159].
Aquatics
Although aquatic exercise has often been recommended for individuals with MS, much of the research employing this therapeutic modality has focused on outcomes of pain, fatigue, cardiorespiratory fitness, gait, and quality of life [160–164]. Research focused on aquatic exercise for improved balance is limited. Nonetheless, significant improvements in standing balance and functional mobility have been shown for individuals with MS following aquatic exercise [165,166]. Similar results on standing balance and functional mobility have also been shown from Ai Chi, a program in which Tai Chi is combined with other techniques and performed standing in shoulder-depth water using a combination of deep breathing and slow, broad movements of the arms, legs, and torso [167]. These methods of intervention, however, still lack evidence from rigorous designs involving control groups and randomization.
Yoga
Yoga has also been explored as a means to improve physical and mental health outcomes in MS. While an initial study showed no significant changes in one-leg stance from an Iyengar yoga program [168], more recent research found Ananda yoga practice effective in improving standing balance [169]. Likewise, other research has shown that static and dynamic standing balance improved after yoga practice, although not significantly better than that from treadmill exercise training [170].
Kickboxing
There has been only one study to date, albeit not an RCT, that has examined kickboxing as a training modality to improve balance in MS. Although kickboxing was found to be a feasible exercise activity, not all participants demonstrated improved balance and mobility outcomes [171]. As such, further investigation of this novel treatment approach is warranted.
Hippotherapy
Hippotherapy has also been employed as a means of balance training because the multidimensional and random nature of the horse’s movement requires the rider to process increased sensory information and make the necessary anticipatory and reactive adjustments for postural control. While one study reported no improvement in postural sway after hippotherapy [172], other research has shown some benefit in balance and gait after riding [173,174]. Although preliminary, findings from 2 of the studies reveal that hippotherapy may be most beneficial for those with primary progressive MS compared to other subtypes of MS [175]. While hippotherapy may have a positive effect on balance in individuals with MS, the data is limited and lacks rigorous examination through randomized controlled study of large samples in order to allow for its advocacy as a primary rehabilitation modality at this time.
What exercise prescription is indicated for Ms. D?
Because Ms. D’s balance deficits have begun to limit her daily functioning and increase her risk of falling, a formal and targeted balance intervention is warranted. Research confirms that exercise would be well tolerated by Ms. D and supports the feasibility of her engaging in various exercise modalities. Although a number of exercise inter-vention studies involving people with MS have been described in the literature, their clinical utility and results in improving balance and mobility are varied. Nonetheless, there is preliminary evidence suggesting that exercise training may have positive effects on balance and functional mobility and could offer Ms. D benefit. This is especially true given that much of the exercise research included individuals with mild or minimal disability and at same stage of disease progression as Ms. D.
Since Ms. D’s balance problems stem from a range of postural impairments across multiple contexts of balance control, her treatment approach must incorporate exercises that include and integrate these underlying control systems. A targeted and multimodal balance exercise program, rather than general physical activity, may be most efficacious toward this end.
Intervention Prescription
Ms. D has poor ability to utilize somatosensory and vestibular inputs in order to dynamically weight the influence of multiple sensory modalities for the control of standing sway under varying sensory conditions. This visual dependence contributes to her poor balance and increases her fall risk when visual inputs are absent (ie, walking in dimly lit rooms) or when optic flow is incongruent or when visual distractions are present (ie, walking in dynamic contexts such as crowded spaces). Ms. D would benefit from exercises requiring greater use of proprioceptive and vestibular inputs, thereby facilitating improved sensory integration. Exercises performed with eyes closed as well as those completed on mats, foam, or other compliant surfaces would be beneficial. She might also benefit from specific vestibular rehabilitation exercises as this approach has resulted in improved sensory integration [143]. Given that Ms. D must regularly concentrate and focus on her balance and consistently look where she is stepping, her balance exercise program should also address her central processing and attentional deficits by including dual-task training [26].
Ms. D also noted that her MS significantly impacts her ability to walk both in terms of effort and distance and adversely affects her participation in social events. Supplemental to her balance exercise program, aerobic exercise, particularly treadmill walking, may offer some benefit both in terms of her endurance as well as gait. While some of the more targeted modalities such as hippotherapy, yoga, and kickboxing have not been extensively studied, they do offer promise and could be used as adjuncts in order to facilitate Ms. D’s motivation and adherence through more diverse programming. Lastly, and although requiring further study, cognitive-behavioral interventions and patient education may be warranted to help Ms. D overcome her fear of falling, low exercise self-efficacy, and any negative beliefs regarding the potential benefits of exercise.
What additional research is needed?
Although valuable insight has been gained from studies of balance and gait impairment with MS, many contexts remain understudied, particularly with regard to understanding both the neuroanatomical and neurophysiologic pathologies that underlie the behavioral impairments of balance and gait in MS. Further, the value of applying this knowledge of balance impairment to clinical diagnostics and prognostics requires further study in order to develop the most cost- and time-effective exams and evidence-based treatment approaches.
Based on the research to date, it remains difficult to draw definitive evidenced-based conclusions regarding what specific exercise mode or training dose would be most beneficial for Ms. D and others with MS. Moreover, while there exists some evidence of efficacious balance outcomes from exercise training, many of the studies involved individuals with mild MS. Only a few studies to date have included those with more advanced disability, thus making prescription generalizations to those more moderately affected by MS tenuous. Irrespective of specific approach, all modalities of balance-oriented interventions require larger controlled studies, inclusion of those with advancing disability status, long-term follow-up, an evaluation of optimal dose or duration, and outcomes on the neural mechanisms of effect.
Summary
Challenges to balance and mobility present serious consequences for those with MS, as falls and fear of falling lead to poor health outcomes and low quality of life. Given that postural impairments result from a diverse set of deficits in different underlying control systems, therapeutic intervention should be multimodal. Exercise prescription should address all affected contexts of postural control, including sensory and motor strategy training during postural transitions as well as induced postural perturbations, strength development, and gait activity. Evidence from clinical trials suggests that targeted balance oriented exercise in people with MS has the potential to improve balance and functional mobility, although more rigorous study on the topic is needed.
Corresponding author: Susan L. Kasser, PhD, Dept. of Rehabilitation and Movement Science, Univ. of Vermont, 306 Rowell Bldg, 106 Carrigan Dr, Burlington, VT 05405, Susan.Kasser@uvm.edu
Financial disclosures: None.