Decreasing Pulmonary Embolism-Related Mortality





Parth Rali, MD
Associate Professor
Temple University Hospital
Philadelphia, PA





Slideshow below.
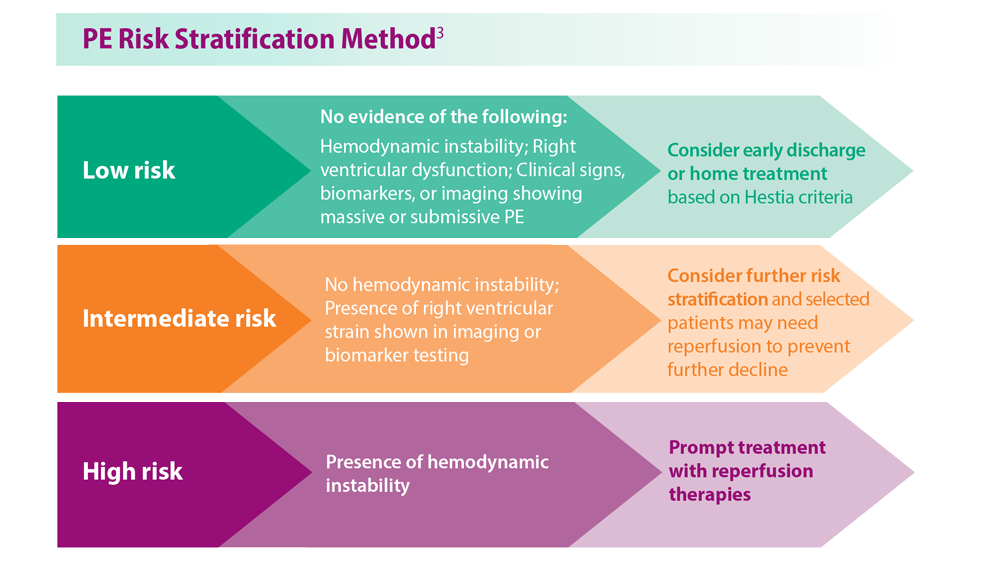
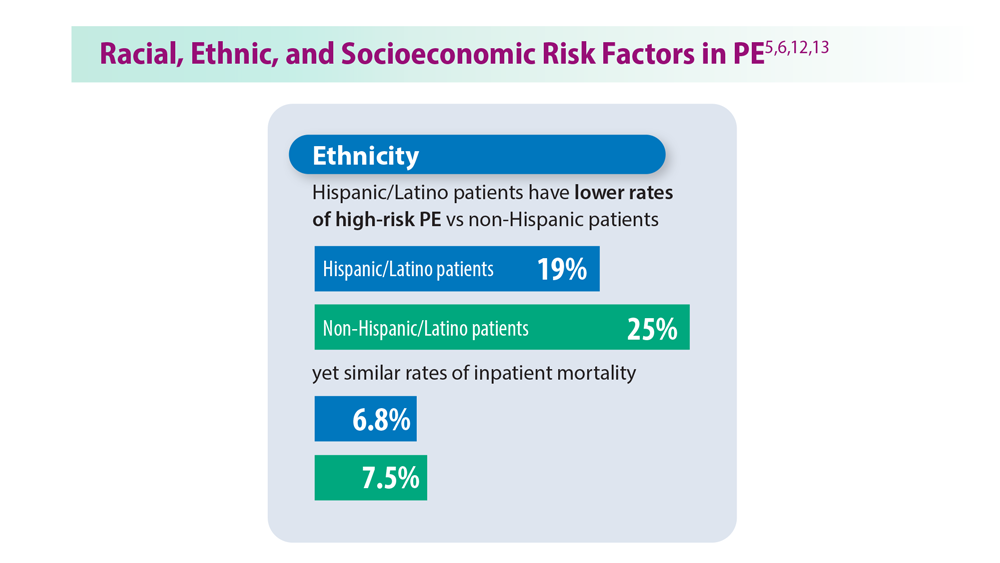
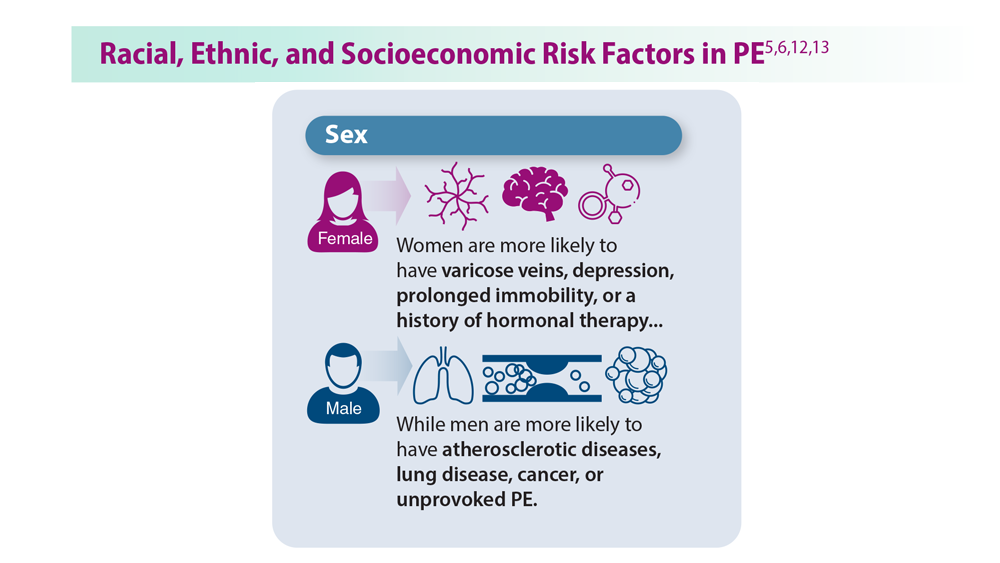
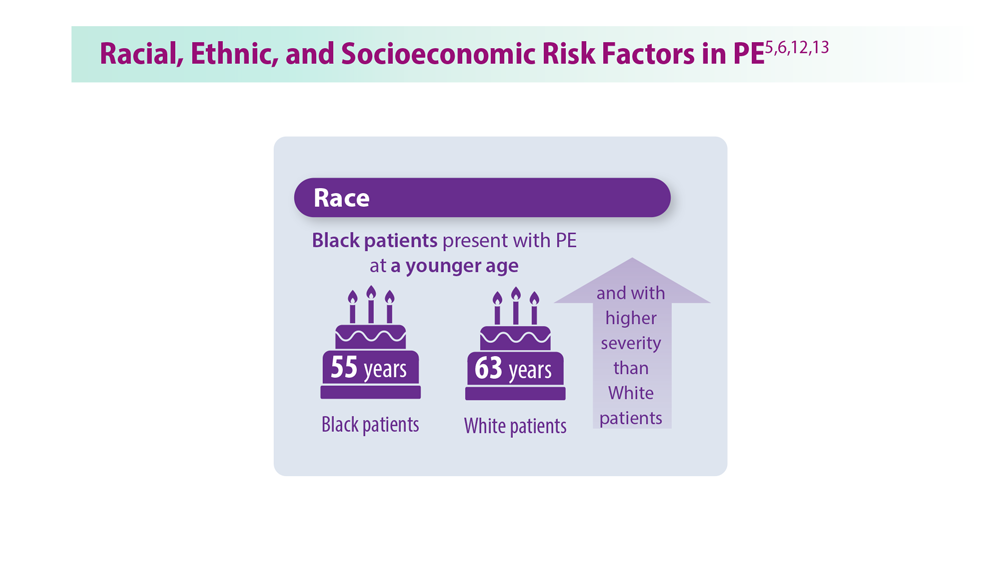
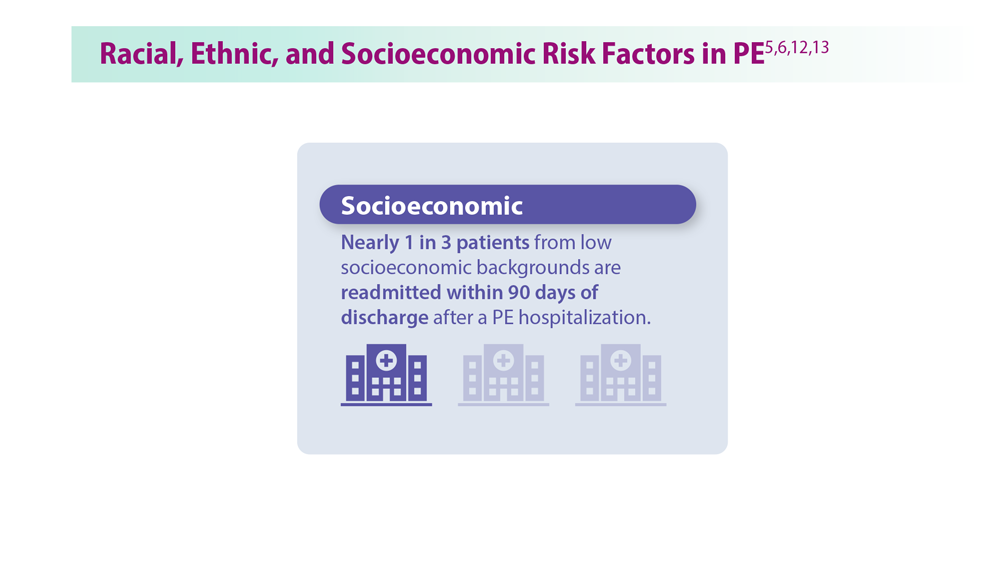
As many as 900,000 patients have deep vein thrombosis (DVT) or pulmonary embolism (PE), also called venous thromboembolism (VTE), each year in the United States, with 100,00 deaths per year.1 In patients with PE, 56% also have DVT, which can affect 30-day mortality rates.2 The field of PE is evolving to help decrease mortality from these events. Proper risk stratification is crucial to identify the best approach for each patient, while the presence of comorbidities and unmodifiable risk factors must also be considered when individualizing care and assessing likelihood of mortality.3,4 As comorbidities increase, mortality increases in PE.4 As well, racial, ethnic, and socioeconomic demographic differences affect PE, with Black patients having greater PE severity and socioeconomically underserved patients having higher follow-up mortality.5,6
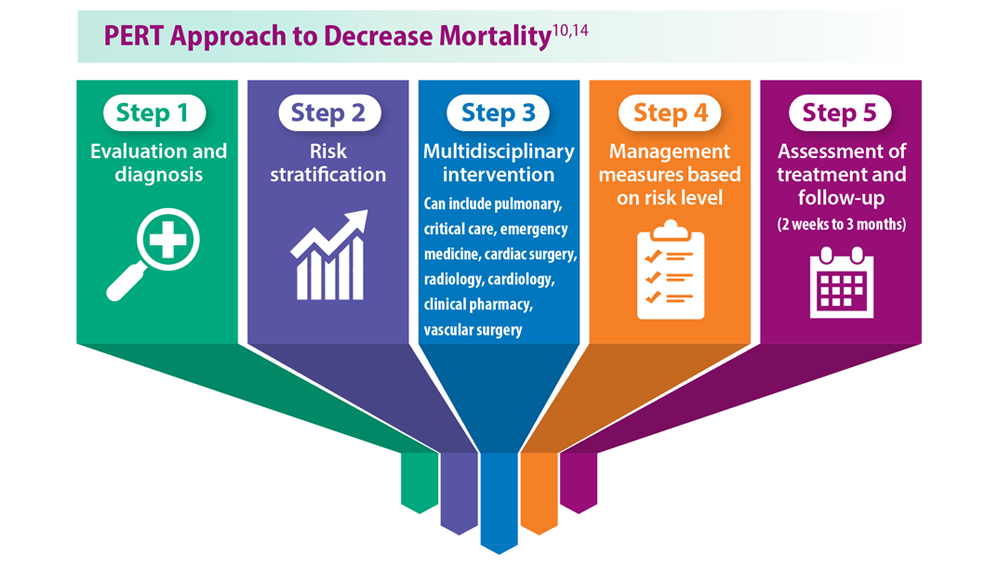
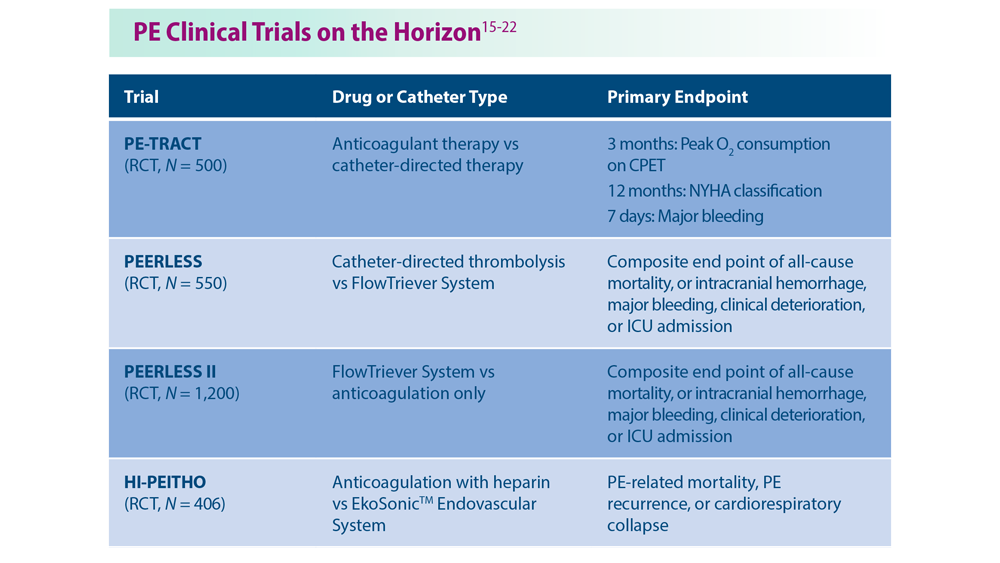
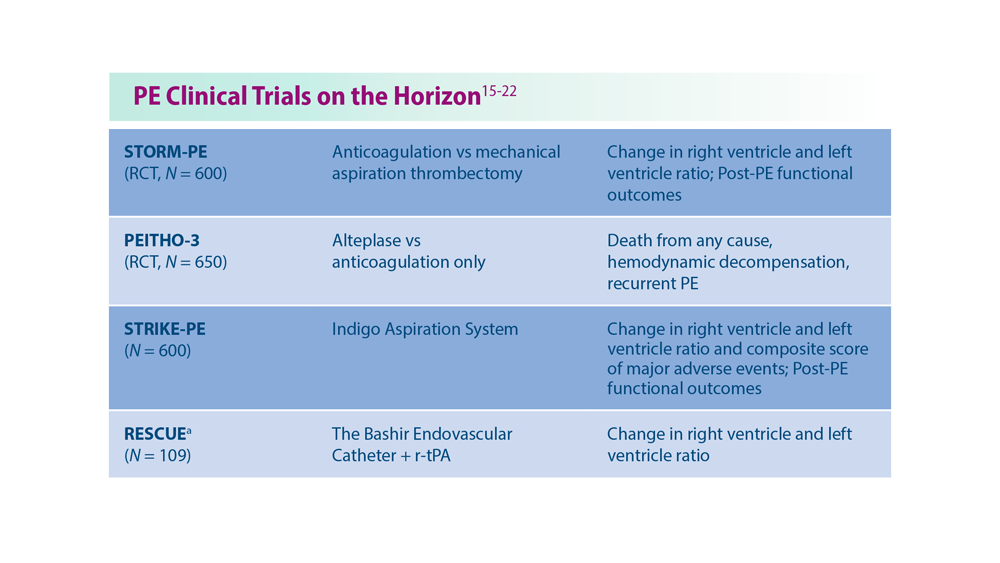
Treatments are also advancing, with many upcoming catheter-based treatments in clinical trials, which have demonstrated rapid recovery of right ventricle function—a primary cause of PE-related mortality.7,8 The effect of catheter-based treatment on long-term functional outcomes is currently being explored in clinical trials. Artificial intelligence is also being used to aid in diagnosis and treatment.9 As the armamentarium of treatment options diversifies, so must our overall approach to management. The PE response team (PERT) strategy uses a multidisciplinary team of experts to further individualize patient care to help decrease mortality and improve follow-up efforts since the post-PE period is a sensitive time for new morbidity.10,11 With proven risk stratification and management strategies available and new treatments on the way, the field of PE looks to improve not only in patient acute mortality, but also long-term functional outcomes, and early detection of post-PE comorbid conditions.