Patterns of care with regard to whole-brain radiotherapy technique and delivery among academic centers in the United States
Background Patterns of practice for whole-brain radiotherapy (WBRT) for the treatment of brain metastases are variable.
Objective To assess patterns of care with regard to WBRT in academic centers in the United States.
Methods A survey of 19 questions was sent to program coordinators at radiation oncology practices accredited by the Accreditation Council for Graduate Medical Education. Coordinators were instructed to send the online survey to resident and attending physicians. We received 95 responses of which 87 were considered complete for analysis. We assessed for association between patterns of care and years in practice (0-5, 6-10, 11-20, and >21 years).
Results A majority of respondents were physicians in practice for ≤5 years (70%). The most frequently used schema for WBRT was 30 Gy in 10 fractions. A majority of patients with radioresistant tumors (52%) were treated with this schema. For radioresistant tumors, those in practice for longer periods more likely to use stereotactic radiosurgery (SRS) alone (P = .027). Younger practitioners ranked the status of extracranial disease for SRS alone as increasingly more important (linear trend, P = .010), and older practitioners ranked histopathology as increasingly more important (linear trend, P = .002).With regard to reirradiation, older practitioners placed more importance on tumor histology (P < .026).
Limitation Contact information was available only for program coordinators.
Conclusions With regard to WBRT, time in practice was the most significant predictor of treatment technique and delivery. Older practitioners placed more importance on tumor histopathology when considering brain irradiation.
Accepted for publication October 24, 2016. Correspondence Parul N Barry, MD; pnbarry@gmail.com. Disclosures The authors report no disclosures or conflicts of interest.
JCSO 2017;15(2):89-94. ©2017 Frontline Medical Communications. doi: https://doi.org/10.12788/jcso.0305.
Despite the recent advances in systemic therapy, metastatic spread to the brain continues to be the most common neurologic complication of many cancers. The clinical incidence of brain metastases varies with primary cancer diagnosis, with estimates ranging from 1.2%-19.8%.1,2 Metastatic spread to the brain is even more prevalent at autopsy, with evidence of intracranial tumor being found in 26% of patients in some series.3 It is possible that the clinical incidence of metastatic disease to the brain will continue to increase as newer therapeutic agents improve survival and imaging techniques continue to improve.
The management of brain metastases has changed rapidly as technological improvements have made treatment increasingly safe and efficacious. Traditionally, treatment consisted of radiotherapy to the whole brain, with or without surgical resection.4,5 More recently, stereotactic radiosurgery (SRS) has been adopted on the basis of evidence that it is safe and efficacious alone or in combination with radiotherapy to the whole brain.6 Further evidence is emerging that neurocognitive outcomes are improved when whole-brain radiotherapy (WBRT) is omitted, which possibly contributes to improved patient quality of life.7 Taking into account this and other data, the American Society for Radiation Oncology’s Choosing Wisely campaign now recommends not routinely adding WBRT to radiosurgery in patients with limited brain metastases.8
Despite this recommendation, many patients continue to benefit from WBRT, and it remains a common treatment in radiation oncology clinics across the US for several reasons. Many patients present with multiple brain metastases and are ineligible for radiosurgery. Even for technically eligible patients, WBRT has been shown to improve local control and decrease the rate of distant brain failure over radiosurgery alone.6 With higher rates of subsequent failures, patients receiving radiosurgery alone must adhere to more rigorous follow-up and imaging schedules, which can be difficult for many rural patients who have to travel long distances to centers. Furthermore, there is some suggestion that this decreased failure rate may result in improved survival in highly selected patients with excellent disease and performance status.9 Controversies exist, however, and strong institutional biases persist, contributing to significant differences in practice. We surveyed academic radiation oncologists and in an effort to identify and describe practice patterns in the delivery of WBRT at academic centers.
,Methods
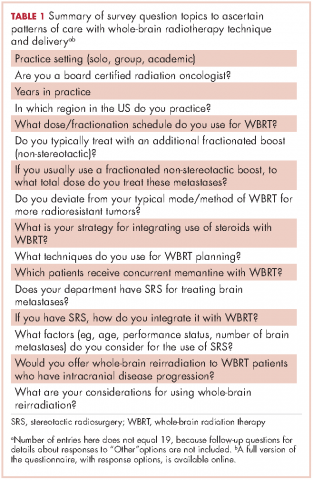
We conducted a thorough review of available literature on radiation for brain metastases and based on our findings, devised a survey 19 questions to ascertain practice patterns and treatment delivery among US academic physicians (Table 1). After obtaining institutional review board approval to do the study, we sent the survey to program coordinators at radiation oncology programs that are accredited by the Accreditation Council for Graduate Medical Education. We instructed coordinators to e-mail the survey to their practicing resident and attending physicians. The surveys were created using SurveyMonkey software. We obtained informed consent from the providers. A total of 3 follow-up e-mails were sent to each recipient of the survey to solicit responses, similar to the Dillman Total Design Survey Method.10
SPSS version 22.0 was used to analyze the data in an exploratory fashion. Statistical methods were used to assess the association of demographic data with SRS and WBRT delivery and treatment technique items when the analyses involved percentages that included the Pearson chi-square statistic and the chi-square test for linear trend. When the analysis focused on ranking data, the Kruskal-Wallis test, Mann-Whitney U test, the Jonckheere-Terpstra and the Kendall tau-b rank correlation were used as appropriate. If there were small sample sizes within some groups, then exact significant levels were assessed. Statistical significance was set by convention at P < .05.
Results
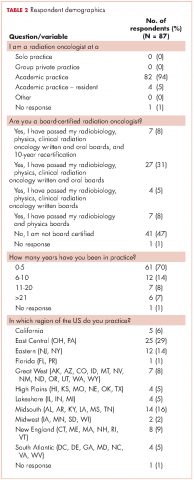
We received 95 responses of which 87 were considered complete for analysis. Forty-seven percent of the 87 respondents were not board-certified, and the remainder had passed their radiobiology and physics boards exams. A majority of respondents (70%, 61 of 87) were physicians who had been in practice for ≤5 years. Fifty-four percent of respondents were located in the Northeast US, 22% in the South, 14% in the West, and 10% in the Midwest and Hawaii (Table 2).