Innovative models of home-based palliative care
ABSTRACTThe focus of palliative care is to alleviate pain and suffering for patients, potentially while they concurrently pursue life-prolonging or curative therapy. The potential breadth of palliative care is recognized by the Medicare program, but the Medicare hospice benefit is narrowly defined and limited to care that is focused on comfort and not on cure. Any organization or setting that has been accredited or certified to provide health care may provide palliative care. Home health agencies are highly attuned to patients’ need for palliative care, and often provide palliative care for patients who are ineligible for hospice or have chosen not to enroll in it. Two home health–based programs have reported improved patient satisfaction, better utilization of services, and significant cost savings with palliative care. Moving the focus of care from the hospital to the home and community can be achieved with integrated care and can be facilitated by changes in government policy.
As the prevalence of serious illness among the elderly population has increased, interest in palliative care has grown as an approach to care management that is patient-centered and focused on quality of life. Case management that employs palliative care has the potential to alleviate unnecessary pain and suffering for patients while they concurrently pursue life-prolonging therapy. Palliative care can be provided across the continuum of care, involving multiple health care providers and practitioners.
Home health care, while often used as a postacute care provider, also can provide longitudinal care to elderly patients without a preceding hospitalization. Home health providers often act as central liaisons to coordinate care while patients are at home, particularly chronically ill patients with multiple physician providers, complex medication regimens, and ongoing concerns with independence and safety in the home.
Home health care can play a critical role in providing palliative care and, through innovative programs, can improve access to it. This article provides context and background on the provision of palliative care and explores how home health can work seamlessly in coordination with other health care stakeholders in providing palliative care.
WHAT IS PALLIATIVE CARE?
Palliative care means patient- and family-centered care that optimizes quality of life by anticipating, preventing, and treating suffering. Palliative care throughout the continuum of illness involves addressing physical, intellectual, emotional, social, and spiritual needs and [facilitating] patient autonomy, access to information, and choice.1
At its core, palliative care is a field of medicine aimed at alleviating the suffering of patients. As a “philosophy of care,” palliative care is appropriate for various sites of care at various stages of disease and all ages of patients. While hospice care is defined by the provision of palliative care for patients at the end of life, not all palliative care is hospice care. Rather, palliative care is an approach to care for any patient diagnosed with a serious illness that leverages expertise from multidisciplinary teams of health professionals and addresses pain and symptoms.
Palliative care addresses suffering by incorporating psychosocial and spiritual care with consideration of patient and family needs, preferences, values, beliefs and cultures. Palliative care can be provided throughout the continuum of care for patients with chronic, serious, and even life-threatening illnesses.1 To a degree, all aspects of health care can potentially address some palliative issues in that health care providers ideally combine a desire to cure the patient with a need to alleviate the patient’s pain and suffering.
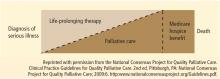
Although the Medicare program recognizes the potential breadth of palliative care, the hospice benefit is relatively narrow. Consistent with the depiction in the Figure,2 the Medicare hospice benefit is limited to care that is focused on “comfort, not on curing an illness”3 (emphasis added). The Medicare hospice benefit is available to Medicare beneficiaries who: (1) are eligible for Medicare Part A; (2) have a doctor and hospice medical director certifying that they are terminally ill and have 6 months or less to live if their illness runs its normal course; (3) sign a statement choosing hospice care instead of other Medicare-covered benefits to treat their terminal illness (although Medicare will still pay for covered benefits for any health problems that are not related to the terminal illness); and (4) get care from a Medicare-certified hospice program.3
There are, however, clear benefits to providing palliative care outside of the Medicare hospice benefit. In particular, patients with serious illnesses may have more than 6 months to live if their illness runs its normal course. Patients who may die within 1 year due to serious illness can benefit from palliative care. Furthermore, some patients would like to continue to pursue curative treatment of their illnesses, but would benefit from a palliative care approach. By providing palliative care in the context of a plan of care with the patient’s physician, the patient and family can comprehensively make decisions and obtain support that enables access to appropriate treatments while allowing enhanced quality of life through symptom management.
WHO CAN PROVIDE PALLIATIVE CARE?
Palliative care can be provided in any care setting that has been accredited or certified to provide care, including those that are upstream from hospice along the continuum of care. Hospitals, nursing homes, and home health agencies can provide palliative care.
The Joint Commission, a nonprofit accrediting organization, currently accredits or certifies more than 17,000 organizations or programs across the care continuum, including hospitals, nursing homes, home health agencies, and hospices. Within the scope of the home care accreditation program, hospices and home health agencies are evaluated by certified field representatives to determine the extent to which their services meet the standards established by The Joint Commission. These standards are developed with input from health care professionals, providers, subject matter experts, consumers, government agencies (including the Centers for Medicare & Medicaid Services [CMS]) and employers. They are informed by scientific literature and expert consensus and approved by the board of commissioners.
The Joint Commission also has a certification program for palliative care services provided in hospitals and has certified 21 palliative care programs at various hospitals in the United States.
The Joint Commission’s Advanced Certification Program for Palliative Care recognizes hospital inpatient programs that demonstrate exceptional patient-and family-centered care and optimize quality of life for patients (both adult and pediatric) with serious illness. Certification standards emphasize:
- A formal, organized, palliative care program led by an interdisciplinary team whose members are experts in palliative care
- Leadership endorsement and support of the program’s goals for providing care, treatment and services
- Special focus on patient and family engagement
- Processes that support the coordination of care and communication among all care settings and providers
- The use of evidence-based national guidelines or expert consensus to guide patient care
The certification standards cover program management, provision of care, information management, and performance improvement. The standards are built on the National Consensus Project’s Clinical Practice Guidelines for Quality Palliative Care2 and the National Quality Forum’s National Framework and Preferred Practices for Palliative and Hospice Care Quality.4 Many of the concepts contained in the standards for inpatient palliative care have their origins in hospice care.
In addition to palliative care accreditation programs, certification in palliative care for clinicians is also possible. The American Board of Medical Specialties approved the creation of hospice and palliative medicine as a subspecialty in 2006. The National Board of Certification of Hospice and Palliative Nurses offers specialty certification for all levels of hospice and palliative care nursing. The National Association of Social Workers also offers an advanced certified hospice and palliative social worker (ACHP-SW) certifcation for MSW-level clinicians. These certification programs establish qualifications and standards for the members of a palliative care team.
Subject to federal and state requirements that regulate the way health care is provided, hospitals, nursing homes, home health agencies, and hospices are able to provide palliative care to patients who need such care.5,6