Obesity Management in the Era of GLP-1 RAs: The Role of GLP-1 RAs





Michael Camilleri, MD, MPhil, DSc
Professor, Department of Medicine,
Pharmacology and Physiology, Division of
Gastroenterology and Hepatology; Consultant
in Gastroenterology and Hepatology,
Mayo Clinic, Rochester, Minnesota
Disclosures: Serve(d) as a member of board for: Phenomix; Received
research grant from: VANDA





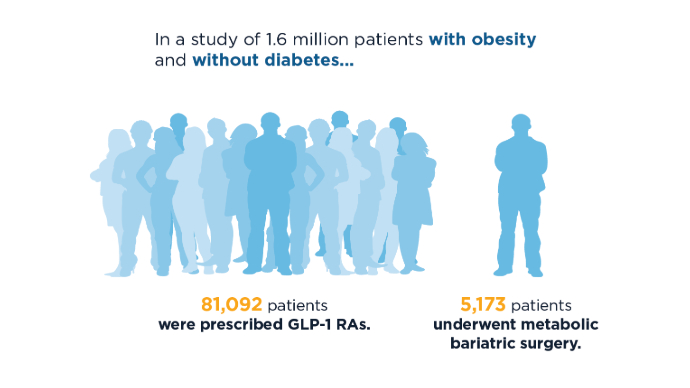
Since 2022, glucagon-like peptide 1 (GLP-1) receptor agonist (RA) use has increased by more than 100%, whereas other obesity interventions, such as bariatric surgery, have decreased.1 There is an ongoing debate on the gastroenterologist’s role in treating obesity.2 Obesity has a profound impact not only on diabetes and cardiovascular and neurologic disease, but also on gastrointestinal (GI) conditions and liver health.2 Thus, obesity is a significant risk factor for other diseases like metabolic dysfunction-associated steatotic liver disease, inflammatory bowel disease, and gastroesophageal reflux disease.
As GLP-1 RA use increases, questions about the risk-benefit profile have arisen, especially among gastroenterologists who assess some of the treatmentrelated GI side effects. GLP-1 RA benefits extend beyond weight loss and diabetes control, improving cardiovascular and neurological outcomes as well.3 However, challenges remain. GLP-1 RAs are associated with delayed gastric emptying, which, though generally manageable, raises concerns about rare complications such as aspiration during procedures.3,4 Despite these concerns, a 2024 study indicates that delayed gastric emptying may normalize in patients over time and rarely, if ever, interferes with clinical practice.3,4 Moreover, for patients with other GI side effects, such as nausea and vomiting, titration adjustments and slower escalation can be helpful.5 According to a review of published data, even though there may be some food retained in the stomach at the time of gastroscopy, the risk for aspiration is extremely low and the examination can usually be completed satisfactorily without having to repeat the endoscopy.3
New multisociety guidelines were released in 2024 on the risk for aspiration in patients on GLP-1 RAs during the periprocedural period, emphasizing balancing benefits of obesity treatment with risks for delayed gastric emptying.6 Although there are many benefits with GLP-1 RAs, questions remain about long-term safety, such as potential impacts on muscle mass and heart health, underlining the need for further research.
 GLP-1 RAs vs Bariatric Surgery: Trends in Use1
GLP-1 RAs vs Bariatric Surgery: Trends in Use1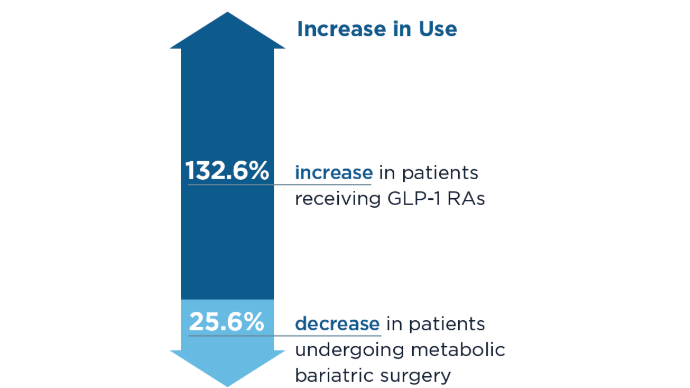 GLP-1 RAs vs Bariatric Surgery: Trends in Use1
GLP-1 RAs vs Bariatric Surgery: Trends in Use1
Between the last 6 months of 2022 and the last 6 months of 2023, there was a significant increase in patients receiving GLP-1 RAs and a significant decrease in patients undergoing metabolic bariatric surgery. Still, less than 6% of patients with obesity in this study received bariatric surgery or GLP-1 RAs, representing a large untreated population. It is unknown if the trend of decreasing bariatric surgery use will stabilize with the high cost and national shortages of GLP-1 RAs.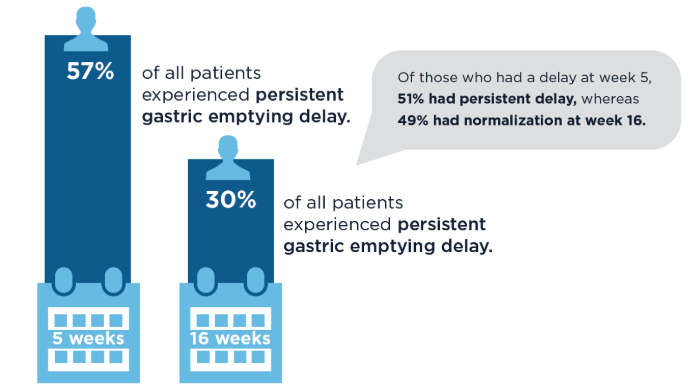 GI Side Effects: Delayed Gastric Emptying4
GI Side Effects: Delayed Gastric Emptying4
Delayed gastric emptying and the risk for aspiration has been a concern in patients taking GLP-1 RAs. However, 2024 data show that in most patients, gastric emptying is unaltered by the GLP-1 RA treatment, or it normalizes over time. Factors that increase risk for delay and resolution remain unclear.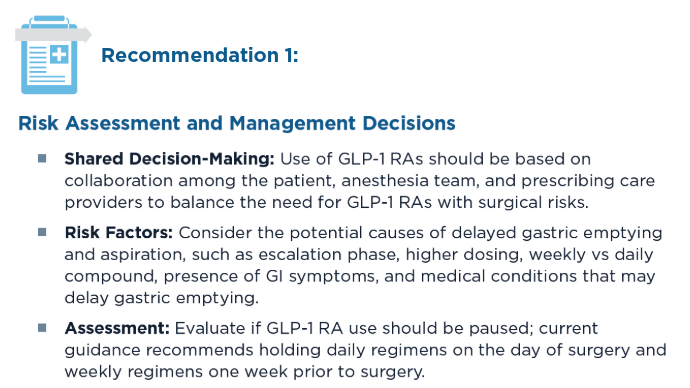 Clinical Guidelines for Perioperative GLP-1 RA Use6
Clinical Guidelines for Perioperative GLP-1 RA Use6
These guidelines have been issued jointly by the American Gastroenterological Association, the American Society for Metabolic and Bariatric Surgery, the American Society of Anesthesiologists, the International Society of Perioperative Care of Patients with Obesity, and the Society of American Gastrointestinal and Endoscopic Surgeons. Clinical Guidelines for Perioperative GLP-1 RA Use6
Clinical Guidelines for Perioperative GLP-1 RA Use6
Recommendations for the use of GLP-1 RAs in the perioperative period are based on clinical practice experience and may change based on expanded research of anti-obesity medications. Liquid diet for 24 hours before the procedure is particularly recommended and seems to have a positive impact in clinical practice. Gastric ultrasound may be clinically limited based on facility resources, interuser variability, and factors such as patient body habitus.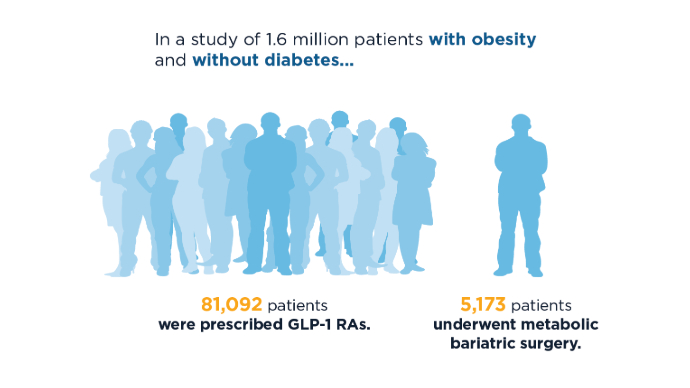 GLP-1 RAs vs Bariatric Surgery: Trends in Use1
GLP-1 RAs vs Bariatric Surgery: Trends in Use1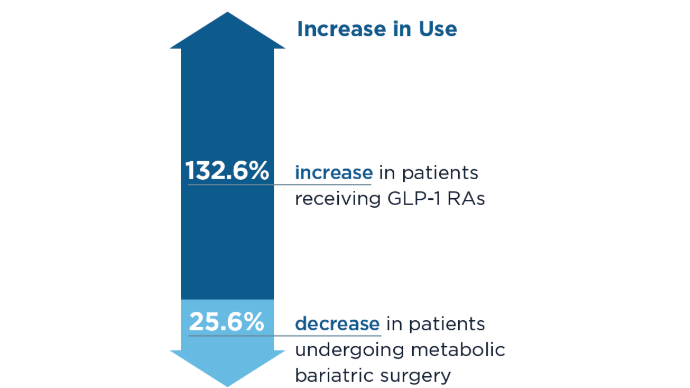 GLP-1 RAs vs Bariatric Surgery: Trends in Use1
GLP-1 RAs vs Bariatric Surgery: Trends in Use1
Between the last 6 months of 2022 and the last 6 months of 2023, there was a significant increase in patients receiving GLP-1 RAs and a significant decrease in patients undergoing metabolic bariatric surgery. Still, less than 6% of patients with obesity in this study received bariatric surgery or GLP-1 RAs, representing a large untreated population. It is unknown if the trend of decreasing bariatric surgery use will stabilize with the high cost and national shortages of GLP-1 RAs.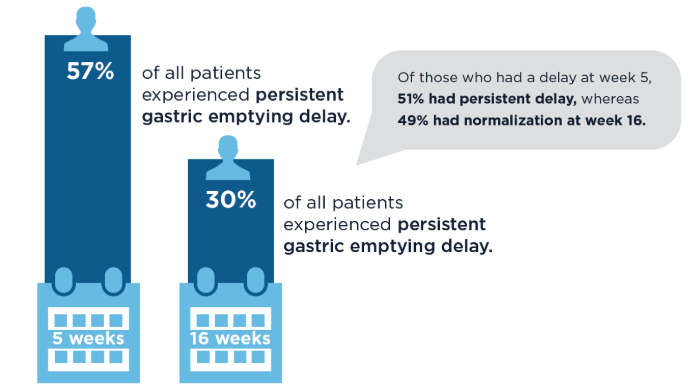 GI Side Effects: Delayed Gastric Emptying4
GI Side Effects: Delayed Gastric Emptying4
Delayed gastric emptying and the risk for aspiration has been a concern in patients taking GLP-1 RAs. However, 2024 data show that in most patients, gastric emptying is unaltered by the GLP-1 RA treatment, or it normalizes over time. Factors that increase risk for delay and resolution remain unclear.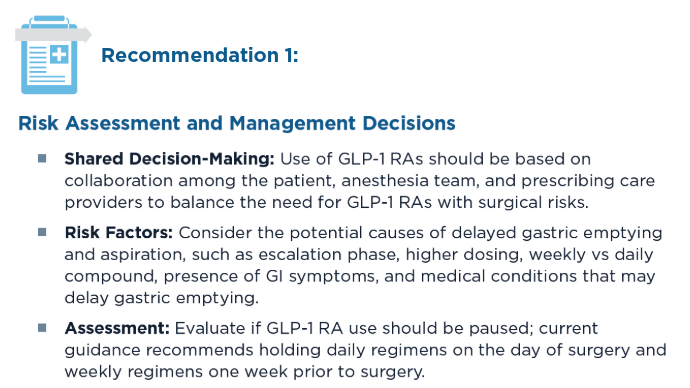 Clinical Guidelines for Perioperative GLP-1 RA Use6
Clinical Guidelines for Perioperative GLP-1 RA Use6
These guidelines have been issued jointly by the American Gastroenterological Association, the American Society for Metabolic and Bariatric Surgery, the American Society of Anesthesiologists, the International Society of Perioperative Care of Patients with Obesity, and the Society of American Gastrointestinal and Endoscopic Surgeons. Clinical Guidelines for Perioperative GLP-1 RA Use6
Clinical Guidelines for Perioperative GLP-1 RA Use6
Recommendations for the use of GLP-1 RAs in the perioperative period are based on clinical practice experience and may change based on expanded research of anti-obesity medications. Liquid diet for 24 hours before the procedure is particularly recommended and seems to have a positive impact in clinical practice. Gastric ultrasound may be clinically limited based on facility resources, interuser variability, and factors such as patient body habitus.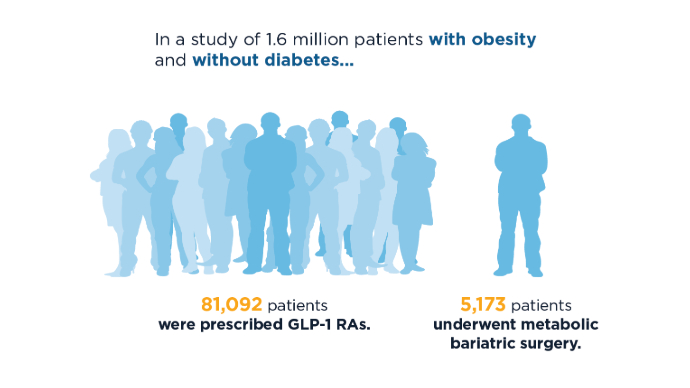 GLP-1 RAs vs Bariatric Surgery: Trends in Use1
GLP-1 RAs vs Bariatric Surgery: Trends in Use1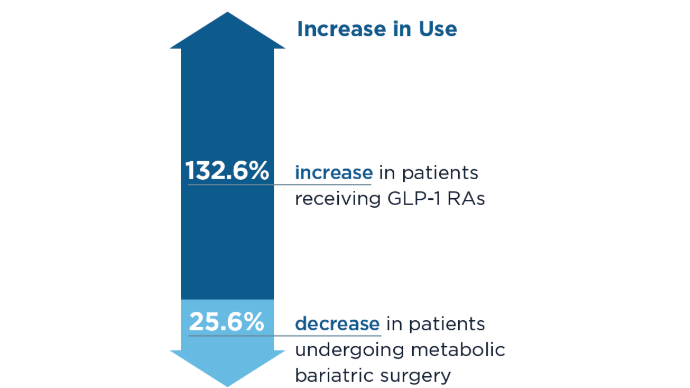 GLP-1 RAs vs Bariatric Surgery: Trends in Use1
GLP-1 RAs vs Bariatric Surgery: Trends in Use1
Between the last 6 months of 2022 and the last 6 months of 2023, there was a significant increase in patients receiving GLP-1 RAs and a significant decrease in patients undergoing metabolic bariatric surgery. Still, less than 6% of patients with obesity in this study received bariatric surgery or GLP-1 RAs, representing a large untreated population. It is unknown if the trend of decreasing bariatric surgery use will stabilize with the high cost and national shortages of GLP-1 RAs.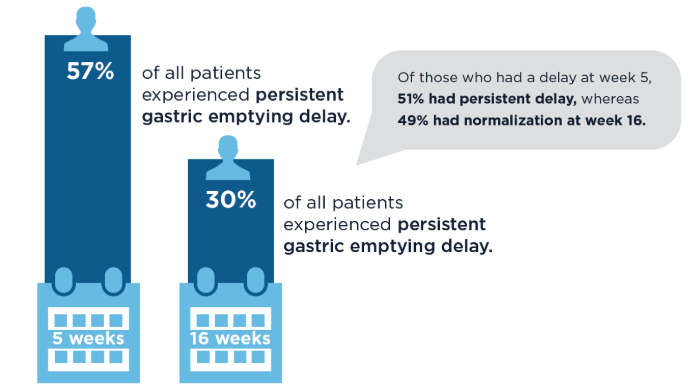 GI Side Effects: Delayed Gastric Emptying4
GI Side Effects: Delayed Gastric Emptying4
Delayed gastric emptying and the risk for aspiration has been a concern in patients taking GLP-1 RAs. However, 2024 data show that in most patients, gastric emptying is unaltered by the GLP-1 RA treatment, or it normalizes over time. Factors that increase risk for delay and resolution remain unclear.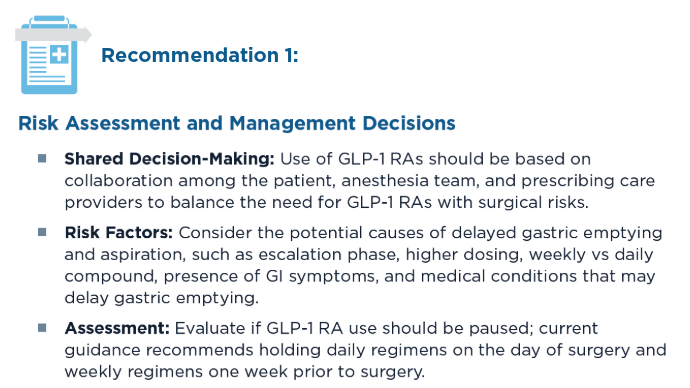 Clinical Guidelines for Perioperative GLP-1 RA Use6
Clinical Guidelines for Perioperative GLP-1 RA Use6
These guidelines have been issued jointly by the American Gastroenterological Association, the American Society for Metabolic and Bariatric Surgery, the American Society of Anesthesiologists, the International Society of Perioperative Care of Patients with Obesity, and the Society of American Gastrointestinal and Endoscopic Surgeons. Clinical Guidelines for Perioperative GLP-1 RA Use6
Clinical Guidelines for Perioperative GLP-1 RA Use6
Recommendations for the use of GLP-1 RAs in the perioperative period are based on clinical practice experience and may change based on expanded research of anti-obesity medications. Liquid diet for 24 hours before the procedure is particularly recommended and seems to have a positive impact in clinical practice. Gastric ultrasound may be clinically limited based on facility resources, interuser variability, and factors such as patient body habitus.
Click to view more from Gastroenterology Data Trends 2025.
,false
