Should the starting age for CRC screening be lowered to 45?
50 is still 50
BY LINDA RABENECK, MD, MPH, FRCPC
CRC screening of women and men aged 50-75 years at average risk has contributed to the overall decrease in the incidence and mortality from the disease in the United States. In 2009, the American College of Gastroenterology recommended that CRC screening among African Americans begin at age 45 years, and a recent study from Kaiser Permanente reported favorable results from FIT screening in this group.1 In 2018 the American Cancer Society surprised the field by releasing an updated recommendation to begin CRC screening in all women and men at age 45 years (Qualified Recommendation). This spring the U.S. Preventive Services Task Force released its updated recommendation to begin screening at age 45 years (B recommendation).2 The rationale for these updated recommendations is based on new information on the epidemiology of the disease in the United States that was incorporated into updated modeling.
What was this new information? An evaluation of time trends in CRC incidence by age group showed that, although the incidence of colon and rectal cancer among those 50 years and older has been decreasing for more than 2 decades, the incidence has been increasing for those younger than 50 years. As important as these CRC incidence trends are to recognize and understand, this does not imply we should start screening everyone in the general population aged 45-49 years. We need to recognize that the absolute increase in CRC incidence in those younger than 50 years is small, that we lack empirical evidence to support such a major change in screening practice, and that we need to consider potential unintended impacts.
When the rise in incidence among younger Americans was first reported there was much discussion about what it meant. It appears that the rise in incidence is a birth cohort effect among people born in the 1960s and subsequent years. Birth cohort effects imply exposures occurring in early life or those experienced by younger generations. Sorting out what these exposures might be is an area of intense research activity currently. Regardless of the drivers of the relative increase in CRC incidence among younger persons, though, it is important to note that the absolute increase is small. What do we mean by this?
As reported by Holli Loomans-Kropp, PhD, MPH, and colleagues,3 for those under age 50 years, the age-adjusted incidence of colon cancer decreased by 0.9% annually from 1980 to 1996, and then increased by 1.3% annually from 1996 to 2016 (Figure 1). 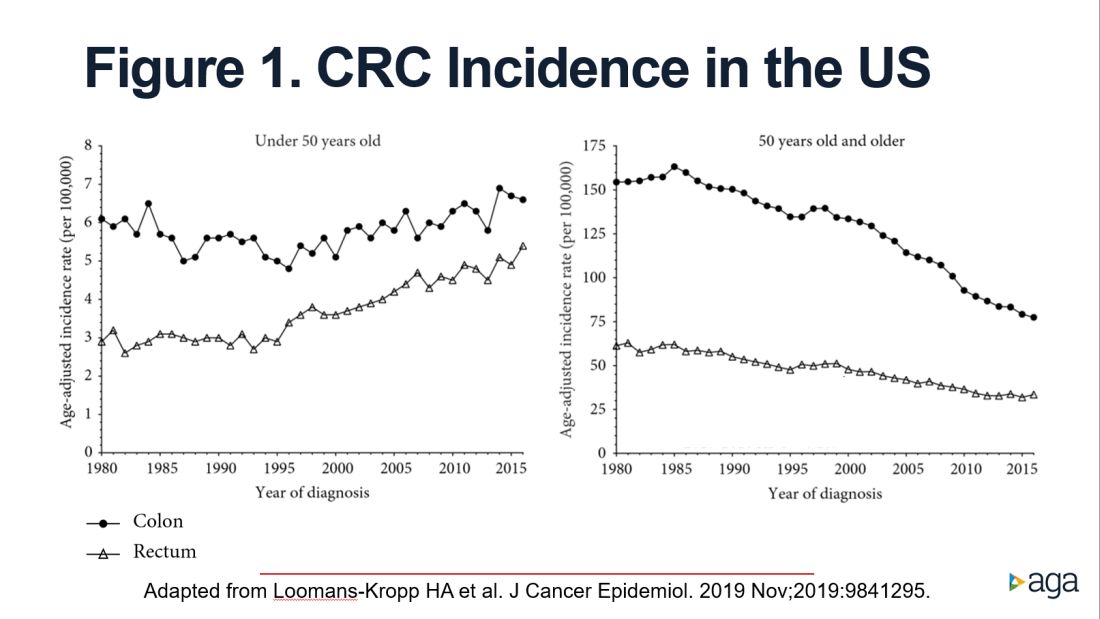
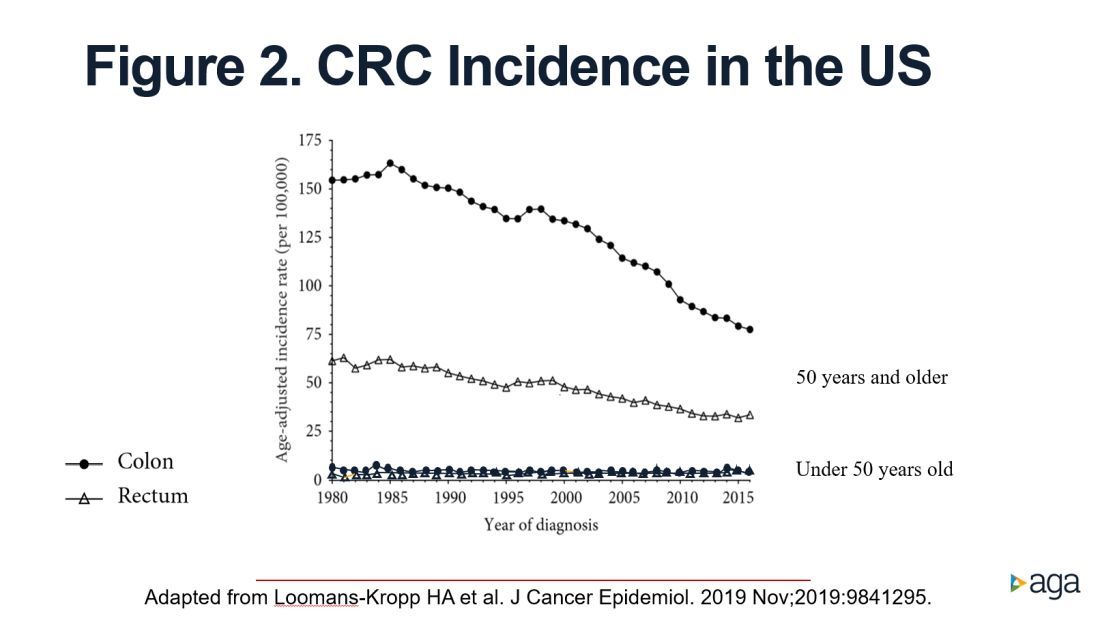
The figure shows that the age-adjusted incidence of rectal cancer among those under age 50 years increased by 2.3% annually since 1991. Figure 1 also shows declines in age-adjusted CRC incidence since 2001 for colon cancer and since 1998 for rectal cancer. However, note the differences in the scales on the Y axes between these two figures. Figure 2 shows this information plotted on the same scale (drawn by hand by author). To recap, these relative increases in incidence are real, but the absolute increases are small.
In addition, not surprisingly, we lack results from randomized controlled trials to support the change in CRC screening recommendation. We are just beginning to see results from other types of study design that seek to address this evidence gap. For example, a recent retrospective cohort study using information recorded in Florida databases evaluated the association between CRC incidence and undergoing colonoscopy at ages 45-49 versus 50-54 years. The authors reported a reduction in CRC incidence in both age groups.4
We also need to consider the resource implications. Lowering the age to start CRC screening to 45 years would expand the target population by greater than 20 million Americans, with all that this entails in terms of additional effort and resources, including colonoscopy. Modeling studies have shown that we would achieve greater clinical benefit with lower cost from directing these colonoscopy resources to those aged 50-75 years who are under/never screened and also ensuring follow-up colonoscopy among those with a positive FIT.5 For example, a study in a U.S. safety-net system reported that among 2,238 patients with a FIT+ followed over 1 year, only 55% underwent a colonoscopy.6
Finally, we need to reflect on existing disparities. If we turn our attention and resources to focus on all those aged 45-49 years in the general population, we risk worsening these disparities.
In conclusion, we need to redouble our efforts to reduce existing disparities in CRC screening participation among those aged 50-74 years and ensure colonoscopy follow-up in those with a FIT+ rather than divert our attention and resources to all those 45- to 49-year-olds who are at lower risk.
Dr. Rabeneck is professor of medicine at the University of Toronto. She has no conflicts of interest.
References
1. Levin TR et al. Gastroenterology. 2020 Nov;159(5):1695-704.e1.
2. U.S. Preventive Services Task Force et al. JAMA. 2021 May 18;325(19):1965-77.
3. Loomans-Kropp HA et al. J Cancer Epidemiol. 2019 Nov 11;2019:9841295.
4. Sehgal M et al. Gastroenterology. 2021 May;160(6):2018-28.e13.
5. Ladabaum U et al. Gastroenterology. 2019 Jul;157(1):137-48.
6. Issaka RB et al. Am J Gastroenterol. 2017 Feb;112(2):375-82.








