Transitioning GI patients from pediatric to adult care
The Transition Readiness Assessment Questionnaire (available online at www.GotTransition.org) is a validated tool that assesses an individual’s awareness of his or her medical needs, treatment plan, and ability to communicate effectively with his or her health care provider.26-28 While not specific to GI disorders, it has been validated in IBD patients and shown to correlate well with the IBD Self-Efficacy Scale for Adolescents.29,30 The University of North Carolina’s TRxANSITION Index, as well as the Social-Ecological Model of Adolescent and Young Adult Readiness for Transition, can be used for patients with various chronic diseases.31,32 Instruments specifically developed to assess transition readiness among patients with IBD include the “IBD-Yourself” questionnaire and MyHealth Passport for IBD.33,34 Additionally, Hait et al. provide a checklist of age-appropriate tasks for patients and their providers.14 The North American Society for Pediatric Gastroenterology, Hepatology and Nutrition has created the “Healthcare Provider Transition Checklist,” which is applicable to all chronic GI disorders.35
Transfer of care
The actual transfer of care is the culmination of the transition process. While the onus of initiating and monitoring a patient’s progress is driven by his or her pediatric provider, a responsive adult provider is integral, so it is vital to identify an adult gastroenterologist ahead of time. This can be especially difficult because most adult gastroenterologists feel uncomfortable about addressing adolescent developmental and mental health issues.36
Local chapters of societies such as the Crohn’s and Colitis Foundation, the American Liver Foundation, and statewide GI societies affiliated with the American College of Gastroenterology, as well as local or regional teaching institutions, are all good resources to identify adult providers interested in a coordinated transition of young adults into their practices. Depending on the availability of a local adult gastroenterologist, one approach to minimize the “growing pains” of transition can be to establish joint clinic visits with pediatric and adult providers; this strategy can help foster trust in the new physician and is generally well-received by patients.37,38 Other institutions may offer alternating visits with adult and pediatric providers during the first year of transition.
Regardless of the manner of the actual transfer of care, it is imperative the adult gastroenterologist be well versed with the natural history and disease complications of the pediatric onset of the specific GI disorder and also appreciate nutrition and concerns regarding growth and radiation. Moreover, they must recognize the convergence and divergence of traditional pediatric and adult care models, as well as the move from a family-centered to an individual-focused environment.39
At the time of the patient’s initial visit, the adult gastroenterologist needs a detailed history of the patient’s disease, a list of past and present medications, the details of any disease- or treatment-related complications or surgeries, and so on. The transfer of relevant medical records is an often overlooked, yet easily remediable, aspect of transfer of care.36 The overall process is best completed by eliciting posttransfer feedback from patients and families after they have established care with the adult provider.
Developing a transition model
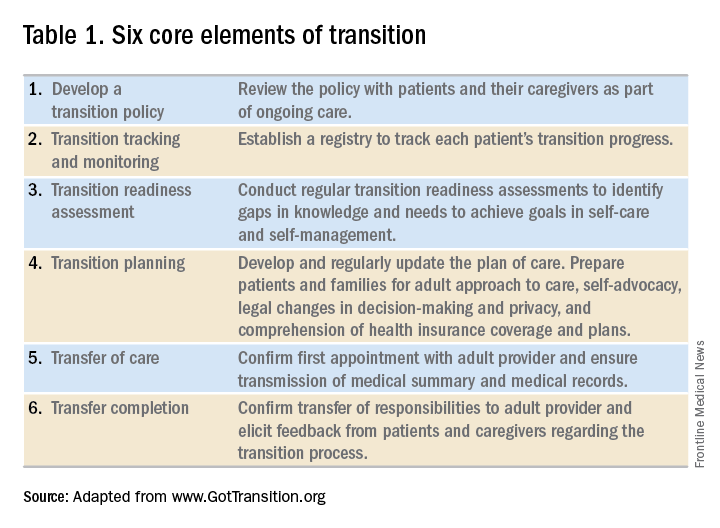
In the absence of standard, disease-specific models of transition, most institutions adapt available resources to develop their own protocols. In 2011, a joint task force of the American Academy of Pediatrics, the American Academy of Family Physicians, and the American College of Physicians published a clinical report on transition. Based on recommendations put forth by the Center for Health Care Transition Improvement – a joint endeavor of the Maternal and Child Health Bureau and the National Alliance to Advance Adolescent Health – the aforementioned task force developed a “Got Transition” model that incorporates six core elements of health care transition (Table 1).
Within the realm of chronic GI disorders, IBD has the most reported data on various models of transition. These include joint adult and pediatric visits, coordinator-initiated transitions, and patient preparation using the assessment tools detailed above. There are no data comparing the efficacy and success of these models and, in the absence of a universally established model for transition in IBD, each institution needs to adopt an approach that best suits the needs of patients and utilizes available resources.
As is the case for patients with IBD, patients with celiac disease need to assume exclusive responsibility for their care as young adults. An important aspect of transition planning for patients with celiac disease is the need to incorporate dietician-led didactic sessions during the transition process. Since patients with celiac disease do not require medications to manage their disease, they are often lost to follow-up as young adults.40 In addition to dietary compliance, it is important to educate young adults about the long-term complications related to celiac disease and the need for regular clinical assessment and monitoring.
Transition of care for patients with EoE is relatively understudied. As EoE was first described only in the 1990s, the diagnosis is still relatively new, and transition programs are limited.41 The natural history and progression of EoE had led to disparate management strategies in adults and children. While the latter are managed with dietary modifications and steroids, adults with EoE often require frequent esophageal dilations because of the increased incidence of fibrosis. In a study of pediatric patients with EoE, most scored lower on transition readiness assessments than did patients with other chronic health conditions.42 Since a majority of patients with EoE require lifelong treatment, they need to be better prepared for transition to adult care.43
In summary, regardless of disease state, transition of care requires planning on the part of the pediatric provider and also close collaboration with patient coordinators, nurses, social workers, and adult providers. While transition is often a complex and lengthy process, it fosters self-reliance and independence among patients while improving their quality of life. Effective communication between pediatric and adult providers as well as patients and families is key to successful transition of care.
Dr. Kaur is the medical director at the Inflammatory Bowel Disease Center and an assistant professor in the section of gastroenterology and hepatology in the department of medicine at Baylor College of Medicine, Houston; Dr. Wyatt is an assistant professor in the section of gastroenterology, hepatology, and nutrition in the department of pediatrics at Baylor.







